Category: Rural Health
Rural Health Clinics with ‘Head-to-Toe and Womb-to-Tomb’ Care
Rural health clinics are safety net providers whose original mandate was primarily to increase access to care for those on Medicaid or Medicare. They provided primary care and perhaps a few other services. But the Rural Health Clinic program has evolved over the years, and some clinics, like Primary Care Centers of Eastern Kentucky, have expanded their roles quite considerably.
‘Grotesque Catch-22’ – Sickest Rural Adults Are the Least Likely to Be Able to Pay for Healthcare
Research on cost barriers to health care found that rural adults were more likely than urban adults to report being unable to pay their medical bills or have problems paying their medical bills. Rural adults also were more likely to use medications in ways not prescribed (like taking pills every other day or only filling prescriptions every other month) to save money on medication.
Struggling to Survive, the First Rural Hospitals Line Up for New Federal Lifeline
Facilities that convert to Rural Emergency Hospital status will get a 5% increase in Medicare payments as well as an average annual facility fee payment of about $3.2 million in exchange for giving up their expensive inpatient beds and focusing solely on emergency and outpatient care. Rural hospitals with no more than 50 beds that closed after the law passed on Dec. 27, 2020, are eligible to apply for the new payment model if they reopen.
Texas Town Tries a New Model for Saving Rural Health Care
The revamped facilities will transfer people who need inpatient care to full-service hospitals nearby. But for many rural communities, such conversions to fewer services will be a bitter pill to swallow.
How primary care is poised to support reproductive health and abortion in the post-Roe era, UW doctors say
Emily M. Godfrey, University of Washington and Adelaide H. McClintock, University of Washington Just over a month after the Supreme Court struck down 50 years of federal protection of abortion rights in the U.S., at least 43 abortion clinics in…
Doctors Trained Abroad Want to See You Now
A handful of states are easing certain licensing requirements, creating programs for foreign-trained doctors to work alongside U.S.-trained ones, reserving residency spots for immigrant health workers and providing help, sometimes including financial aid, for those working to get a U.S. license. States hope the efforts can not only get medical providers to more places where they are needed—particularly underserved rural and urban areas—but also lead to more professionals who speak the same language as and are culturally attuned to those they treat in an ever more diverse America.
Biden’s Vaccine Mandate Could Further Strain Rural Hospitals
But the story may be more complicated in rural America, where resistance to the vaccine remains strongest. Some rural hospital leaders worry the vaccine mandate will exacerbate a labor shortage that was profound even before the pandemic. There are predictions that some hospitals will have to close their doors.
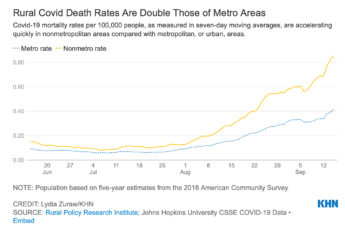
Covid Is Killing Rural Americans at Twice the Rate of Urbanites
Rural Americans are dying of covid at more than twice the rate of their urban counterparts — a divide that health experts say is likely to widen as access to medical care shrinks for a population that tends to be older, sicker, heavier, poorer and less vaccinated.
Rural Hospitals Can’t Find the Nurses They Need to Fight COVID
Across the country, thousands of hospitals are overwhelmed with critically ill patients, prompting many overburdened nurses to change careers or retire early. The shortages are particularly dire in rural areas, rural health experts say, because of the aging workforce and population, smaller salaries and intense workload.
Influx of Medical School Students Could Overwhelm Montana Resources, UW Leaders Warn
Opening two new medical schools in Montana would stretch and possibly overwhelm the state’s physicians who provide the clinical training that students need to become doctors, UW leaders say.
What the Slowing Vaccine Rates Mean for One Rural Montana County
Daily covid vaccination rates are falling nationwide. Gaps in vaccine uptake are starting to show, especially in rural America. That leaves many communities grappling with an imperfect pandemic endgame.
Riding Herd on Mental Health in Colorado Ranching Country
Two-thirds of farmers and farmworkers say the pandemic has impacted their mental health.
Fewer rural students applying to medical school
This decrease could lead to fewer doctors in less populated areas of the country
These States Found the Secret to COVID-19 Vaccination Success
Centralized approaches by states like West Virginia and Alaska have proved to be more efficient.
How the CARES Act Forgot America’s Most Vulnerable Hospitals
CARES Act funding for health care providers has been plagued by a dizzying rollout and, at times, contradictory guidelines for how to use the funding.