COVID: lambda variant is now in 29 countries, but what evidence do we have that it’s more dangerous?
Tara Hurst, Birmingham City University
Peru has the highest number of COVID deaths per capita, by far. For every 100,000 of the population, 596 have died of COVID. This is almost double the next hardest-hit country, Hungary, which has 307 deaths per 100,000 people.
There are many reasons Peru has fared so badly in the pandemic. They include a poorly funded, under-prepared healthcare system with too few ICU beds; slow vaccine rollout; limited testing capacity; a large informal economy (few people could afford not to work); and overcrowded housing. The country was also beset by the lambda variant. Initially reported in the capital, Lima, in August 2020, by April 2021 it accounted for 97% of all sequences in Peru.
Lambda has now gone globetrotting. According to a recent World Health Organization (WHO) report, it has been found in 29 countries. The report states: “Lambda has been associated with substantive rates of community transmission in multiple countries, with rising prevalence over time concurrent with increased COVID-19 incidence.”
On June 14 2021, WHO declared lambda a “global variant of interest”. Public Health England followed suit on June 23, designating it a “variant under investigation” because of its “international expansion and several notable mutations”.
Of the eight confirmed cases of lambda in the UK, most have been linked to overseas travel.
What the evidence shows
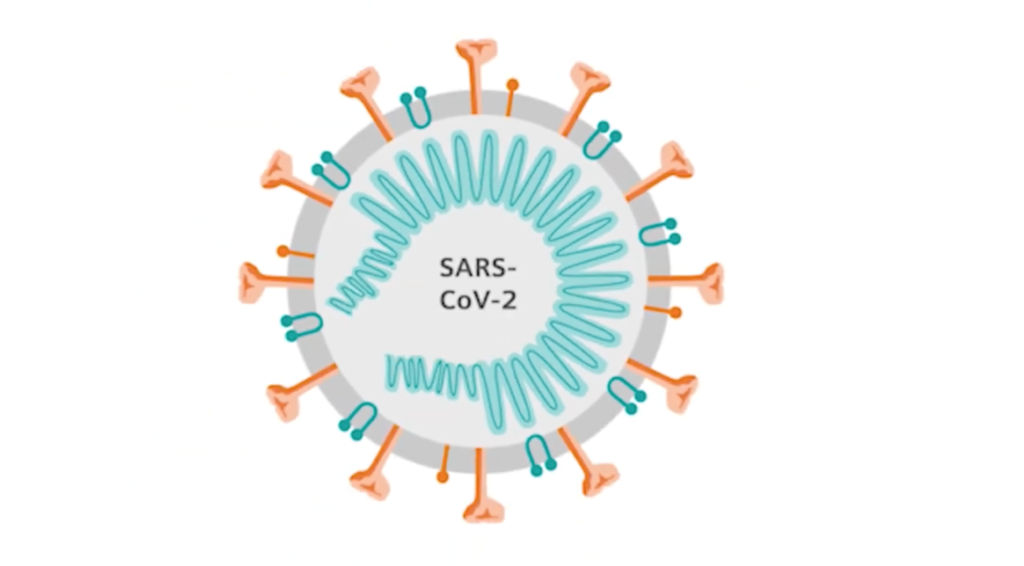
A variant of interest is one that has mutations that are predicted or known to affect things such as transmissibility (how easily the virus spreads), severity of disease, ability to evade immunity from past infections or vaccines, or confound diagnostic tests.
Many scientists speak of lambda’s “unusual combination” of mutations, which may make it more transmissible.
Lambda has seven mutations on the spike protein, the mushroom-shaped projections on the outer shell of the virus that help it latch onto our cells and invade them. These mutations may make it easier for lambda to bind to our cells and make it harder for our antibodies to latch onto the virus and neutralise it. https://www.youtube.com/embed/OVDaq_vOQ48?wmode=transparent&start=0
But it’s important to remember that neutralising antibodies aren’t the only tool in the immune system’s toolkit – they are merely the easiest to study. T cells play a vital role too, so a handful of mutations – however unusual – might not be enough to allow lambda to dodge our immune system altogether.
So what evidence do we have that these mutations make lambda more dangerous than the original coronavirus? Very little, it turns out.
There are no published studies on the lambda variant and just a handful of preprints – papers that have yet to be subject to the scrutiny of other scientists (peer review) and published in a journal.
A preprint from the New York University Grossman School of Medicine looked at the effect of the Pfizer and Moderna vaccines against the lambda variant and found a two-to-threefold reduction in vaccine-elicited antibodies compared with the original virus. In the scheme of things, this is not a massive loss of neutralising antibodies. The researchers conclude that these mRNA vaccines will probably remain protective against the lambda variant.
Researchers from the University of Chile investigated the effect of the Sinovac (also known as “CoronaVac”) vaccine against the lambda variant. They also found a threefold reduction in neutralising antibodies compared with the original variant.
The fact that these two studies found that neutralisation is at least partially retained is promising, not least because this is only one facet of the immune response elicited by vaccination.
According to PHE’s latest “risk assessment” (July 8) of lambda, there is no evidence of a country where lambda has outcompeted delta. Studies are ongoing, but for now, lambda remains a variant of interest rather than a variant of concern.
Tara Hurst, Lecturer, Biomedical Science, Birmingham City University
This article is republished from The Conversation under a Creative Commons license.
Read the original article.