Eileen Crimmins, University of Southern California and Jessica Faul, University of Michigan
Can we objectively tell how fast we are aging? With a good measure, scientists might be able to change our rate of aging to live longer and healthier lives. Researchers know that some people age faster than others and have been trying to concisely measure the internal physiological changes that lead to deteriorating health with age.
For years, researchers have been using clinical factors normally collected at physicals, like hypertension, cholesterol and weight, as indicators to predict aging. The idea was that these measures could determine whether someone is a fast or slow ager at any point in their life cycle.
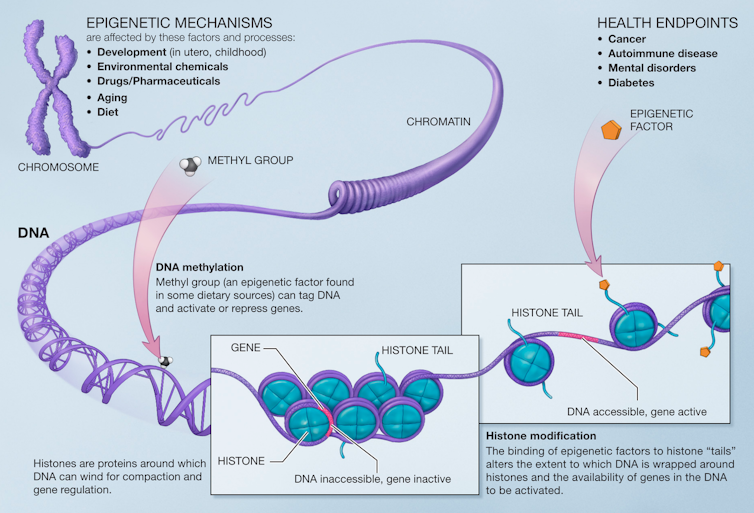
But more recently, researchers have theorized that there are other biological markers that reflect aging at the molecular and cellular level. This includes modifications to a person’s genetic material itself, or epigenetics.
While each person has a genetic makeup that largely does not change over their lifetime, chemical changes to their genetic material that occur throughout life can change which genes are turned on or off and lead to more rapid aging.
These changes typically involve the addition of methyl groups to DNA and are influenced by social and environmental exposures, such as adverse childhood experiences, smoking, pollution and depression.
But how well do epigenetic markers predict the important health changes that happen with aging? We are social scientists who study how social factors predict aging. Our previous research has shown that factors like education, poverty, race, access to medical care and certain health behaviors can influence aging rates.
We are incorporating biological measures like epigenetic age in large population studies to understand how social factors get “under the skin” and affect aging. In our recently published study, we found that while epigenetic age does predict certain health outcomes later in life, it does little to explain important differences related to social factors.
What is epigenetic aging?
In 2013, geneticist and biostatistician Steve Horvath introduced the idea that a person’s rate of aging would be captured by the level of methylation in their genome. He also developed ways to measure epigenetic age in terms of years and compare this age to one’s chronological age.
Researchers have since developed several measures that can more reliably predict health outcomes based on epigenetics. Some have suggested that DNA methylation could potentially be used to summarize the amount and rate of aging with a few drops of blood.
Comparing epigenetic and social factors
It has been unclear how well epigenetic age predicts health outcomes compared to other nongenetic factors like demographics and socioeconomic status. We wanted to see whether epigenetic age, measured by DNA methylation levels in the blood, predicted four aging-related health outcomes: death, chronic disease, physical disability and cognitive dysfunction.
Using data from the Health and Retirement Study, a large, nationally representative sample of Americans over the age of 56, we found that epigenetic age predicted all of the health outcomes we examined. Epigentic age most strongly predicted death and morbidity later in life. So overall, people with a higher epigenetic age experienced poorer health.
On the other hand, epigenetic age did not explain why people with certain demographics – such as having less education, smoking, being Black or Hispanic, being obese or having a more difficult childhood – experienced worse health outcomes earlier or more frequently. These social factors were able to predict mortality and morbidity just as well as epigenetics and substantially predicted physical and cognitive functioning better than epigentic age.
Our findings suggest that while DNA methylation is a useful addition to the toolbox to predict health outcomes later in life, other factors such as demographics, socioeconomic status, mental health and health behaviors remain equally, if not more robust, predictors of health.
Better predicting aging and health
Epigenetic aging processes like DNA methylation show promise in explaining aging. But there is still a long way to go before researchers fully understand the molecular and cellular mechanisms underlying aging.
Improving our ability to measure both the lifetime social experiences that affect biology and the biological mechanisms that underlie aging could lead not only to better measurements of aging, but to better treatments and disease prevention for those who need it the most.
Eileen Crimmins, Professor of Gerontology, University of Southern California and Jessica Faul, Research Associate Professor of Epidemiology, University of Michigan
This article is republished from The Conversation under a Creative Commons license.
Read the original article.