Simon Sherry, Dalhousie University
Eating disorders such as anorexia nervosa, bulimia nervosa and binge eating disorder are serious health risks, and can be life-threatening. They are also common, especially among teenage girls.
More than 100,000 Canadians over the age of 15 are diagnosed with an eating disorder each year. Onset usually occurs between ages 14 and 19. In fact, eating disorders are the third most common chronic illness among teens.
Adolescence is also when eating disorders have the greatest negative effects on health. Five per cent of the general population in North America will suffer from an eating disorder in their lifetime, but few people seek treatment. The prevalence of eating disorders and struggles to access help highlight the need to increase awareness and decrease stigma.
Causes and risk factors
The greatest risk factor for eating disorders is sex. Eating disorders occur 10 times more often in females than in males. However, genetic, biological, psychological and cultural factors all affect the development of an eating disorder.
- Genetics: Specific genes have been linked to anorexia and bulimia, and studies of twins suggest eating disorders are very heritable genetic diseases, with rates estimated between 50 per cent and 83 per cent. People may be more likely to inherit an eating disorder if their mother was exposed to stressors or complications shortly before or after birth.
- Biology: Biological factors such as abnormalities in brain structure or chemistry can cause eating disorders. Developmental disorders such as autism or ADHD affect one-fifth of those with anorexia. Mood disorders such as depression or anxiety are associated with binge eating disorder and bulimia.
- Psychology: Eating disorders are more common in people with perfectionism, obsessive compulsive traits, avoidant coping methods and anxiety. People who often have negative emotions, low self-esteem and who worry or stew on those problems are at risk of eating disorders, as are people who are dependent and sensitive to failure. Individuals with body dysmorphic disorder (who obsess over perceived flaws in their body) are also likely to develop eating disorders.
- Society and culture: Eating disorders are more common in cultures that value thinness. Societies with unrealistic body ideals (both in shape and size) encourage people to negatively compare their body to others and have poor self-esteem. Those societies also encourage a culture of criticism and bullying around weight. Abuse, neglect or general adversity increases the risk of developing an eating disorder.
Unfortunately, eating disorders can be self-propelling. Eating disorders change the way you perceive food and body shape. Starvation also shrinks the brain and causes problems such as rigidity, emotional dysregulation and social difficulties that maintain the illness. The effects of starvation are particularly exaggerated during adolescence because it is a period of growth and vulnerability.
Health effects
Eating disorders are chronic, distressing and impede one’s ability to function. They increase risk of depression, anxiety disorders, obsessive compulsive disorders, personality disorders, substance abuse, morbidity and future obesity.
People with eating disorders are six times more likely to die than the general population, and five times more likely to attempt suicide. In fact, anorexia has an especially high mortality rate compared to other psychiatric illnesses.
Eating disorders can also have consequences later in life because of their effects on the skeleton (for example, growth retardation and osteoporosis), reproductive system and brain.
- Anorexia nervosa
People with anorexia experience hormonal changes, heart problems, electrolyte imbalances, decreased fertility, loss of bone density, anemia and suicidal ideation. Some of these effects can be deadly.
Without enough calories, the body is forced to slow its processes to conserve energy. As such, people with anorexia often complain of stomach cramps, constipation, acid reflux, slow heart rate, swelling in extremities, menstrual irregularities, difficulty functioning, dizziness, sleep disturbances and impaired immunity and healing.
Nutritional deficits can cause dental problems, dry skin, dry and brittle hair and nails, thinning hair and muscle weakness.
People with anorexia are often cold and develop fine hair on their body to help conserve heat. They are also often hyperactive (exercise too much), and if so, can suffer higher relapse rates, younger age of onset, more severe psychopathology, lower BMI, higher dissatisfaction with their body and lowered response to treatment.
- Bulimia nervosa
Since bulimia is characterized by periods of both binge eating and periods of purging or starvation, people with bulimia experience many of the same consequences of anorexia. In addition, they often have noticeable changes in weight or experience fluid retention.
As a result of induced vomiting, they may have cuts and calluses across the top of finger joints, swelling around salivary glands, esophagus damage and cavities or tooth discoloration.
Bulimia is associated with self-harm, substance abuse, miscarriages, suicide and impulsive behaviours.
- Binge eating disorder
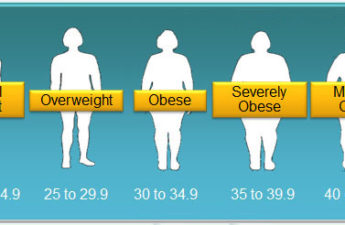
People with binge eating disorder often suffer from weight stigma, noticeable cycles of weight changes, clinical obesity and depression. They are nearly twice as likely to become overweight or obese compared to the general population, and have double the risk of developing severe depression.
Treatment
Despite how common, chronic and challenging eating disorders are, few people seek treatment. Treatment is effective, though. Many behavioural, psychological and physical effects of starvation clear up once weight is gained and brain mass restored.
For anorexia, an approach that tackles medical, nutritional, social and psychological aspects is recommended. For bulimia and binge eating disorder, cognitive behavioural therapy (which involves identifying, challenging and changing unhelpful thought patterns) has been shown to be effective, as has medication such as the stimulant Vyvanse (lisdexamfetamine).
Eating disorders are serious conditions that can endanger health, but there are effective treatments. There is hope. Increasing awareness of eating disorders helps break the stigma and encourages people to get help.
This is a corrected version of a story originally published on Feb. 28, 2023. The earlier story stated the mortality rate for anorexia was approximately 10 per cent. It now states that anorexia has an especially high mortality rate compared to other psychiatric illnesses.
Simon Sherry, Clinical Psychologist and Professor in the Department of Psychology and Neuroscience, Dalhousie University
This article is republished from The Conversation under a Creative Commons license.
Read the original article.