Public Health Insider, Public Health — Seattle & King County
August 25, 2017
In response to questions about hospital related infections and the outbreak of bacterial infections at the downtown campus of Virginia Mason Franciscan Health Medical Center (VMMC), we are providing answers to some common questions.
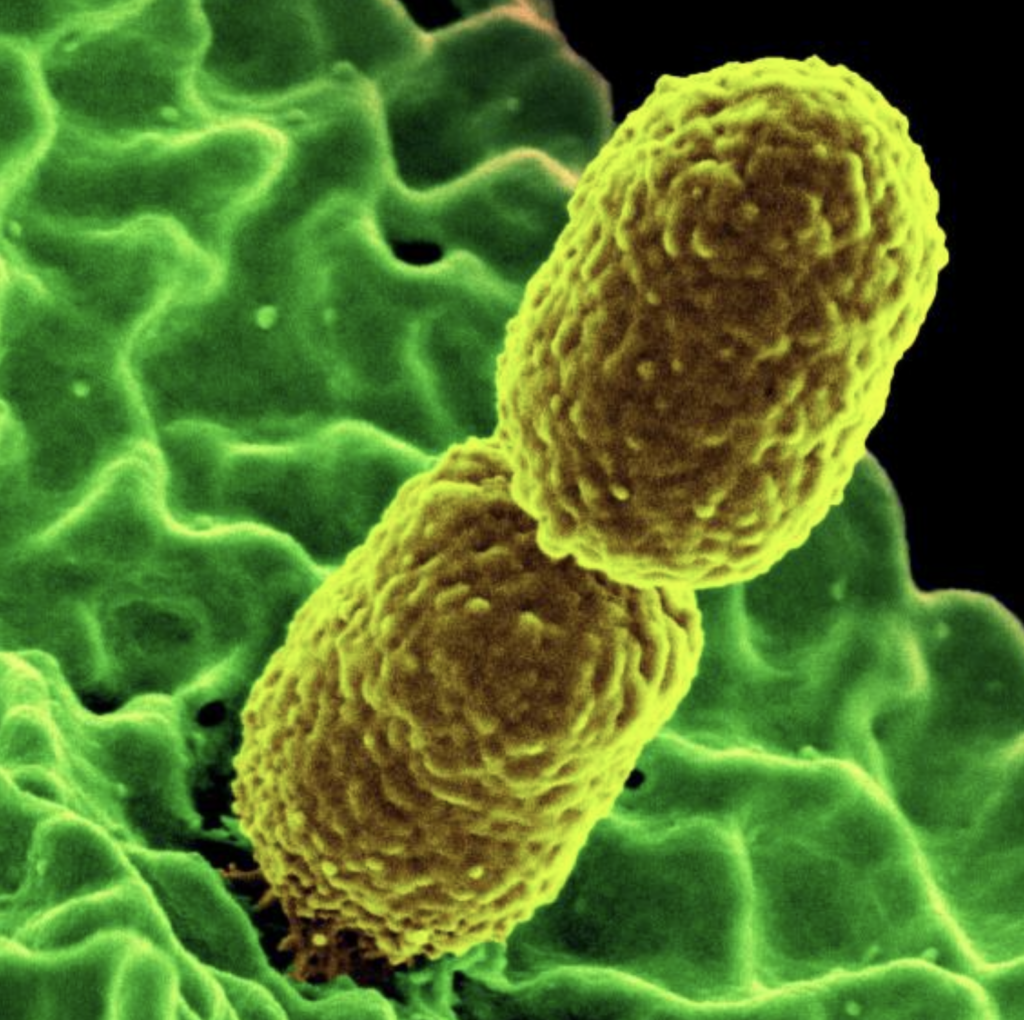
First, what is Klebsiella [kleb−see−ell−uh] and how does it spread?
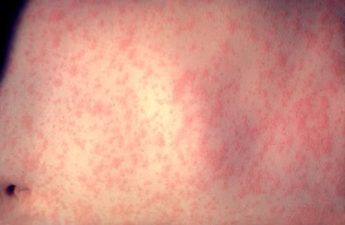
Klebsiella pneumoniae are common bacteria that can be part of the normal bacteria living in our bodies, including in our intestines. However, sometimes the bacteria can enter a part of the body where it is not normally found and can cause infections such as urinary tract infections, surgical site infections, and pneumonia.
A person’s risk of infection depends on a number of different factors which may include procedures they have had or whether they have a weakened immune system. Klebsiella bacteria don’t spread through the air. In healthcare settings, the bacteria can spread through person-to-person contact, often from contaminated hands. This can happen if you touch someone who has the infection and don’t wash your hands well afterward. Additionally, the bacteria might contaminate environmental surfaces, such as medical equipment like ventilators or catheters. Bacteria can then spread from the equipment to the patient.
How is it treated?
Providers often treat Klebsiella infections with antibiotics. But sometimes bacteria can be difficult to treat. Over time, Klebsiella and other types of bacteria have been finding ways to resist antibiotics normally used for treatment. The strain of bacteria identified in the recent infections at VMMC are resistant to some but not all antibiotics. If you have a drug-resistant infection, a healthcare provider will order lab tests to determine which antibiotic will work best for you.
Why is public health concerned about an outbreak of this bacteria?
One of the reasons Public Health is concerned when these bacteria circulate is because it has a specific enzyme that breaks down common types of antibiotics, making them ineffective. While this strain is resistant to certain antibiotics, there are other antibiotics that can be used in these situations (such as antibiotics called carbapenems) that are still effective.
How is it prevented?
Public Health works with hospitals to monitor increases in bacteria or other organisms to help prevent broader spread of infection. To help prevent the spread of bacteria between patients, hospitals follow careful cleaning procedures along with other infection-prevention practices, and healthcare staff need to use strict hand hygiene practices. Some procedures may also require specific steps to be taken to ensure it is conducted in a sterile fashion. Healthcare staff take steps to minimize the risk of infection in these situations. Healthcare facilities have also taken steps to monitor increases in infection.
When did this outbreak start?
Cases of Klebsiella associated with this outbreak were identified starting in October 2022 through a process known as genomic sequencing or “fingerprinting” to show how bacteria are related to one another. It’s important to note that hospitals normally see a certain number of Klebsiella and other bacterial infections—their baseline–as they conduct laboratory surveillance because they are common. Hospitals report to public health when they see an increase from their baseline rate or other evidence of a suspected healthcare-associated outbreak.
How large is the outbreak and how severe is it?
Case information can be found on VMMC’s community update webpage. As of 4/28/23, Public Health was notified by VMMC of 31 cases and 7 people who had died since the outbreak began. The data being tracked, including case numbers and outcomes, are not usually real-time. For example, collected samples requiring further specialized testing may be done in groups which can delay test results. During an investigation, these data fluctuate and an increase in reported numbers does not mean that those cases are new infections. Due to the medical complexity of these patients, there may be multiple possible causes of death for those individuals who died after the Klebsiella infection was diagnosed.
This infection has impacted people who at one point were hospitalized for other medical conditions, some many months ago. Therefore, it is unfortunately expected that some of these people will have since passed away. What is most important is that healthcare staff and hospitals continue to improve infection prevention and control processes and remain vigilant given how common these bacteria are.
For updated information on cases, visit the Virginia Mason Medical Center community resources page.
What is the risk to patients of getting this type of infection at hospitals, including at Virginia Mason?
Risk of acquiring infections in any hospital or during a procedure is always present. To reduce risk of infection, infection prevention teams in hospitals take steps every day to lower that risk through preventative measures. This includes hand hygiene, environmental cleaning and ensuring certain procedures are performed under sterile conditions.
It’s a positive sign that over the course of the investigation, the number of patients who have the associated Klebsiella outbreak strain has decreased.
What do we know about the source of the outbreak and recommendations for the hospital?
We have not identified a source and may never do so. We continue to consult with CDC, however, there are many reasons why source identification can be difficult.
There is no clear incubation period for this type of infection, so people can have Klebsiella bacteria without showing symptoms for a long time (weeks to months), making it very difficult to identify where and when someone may have been infected.
Patients with medically complex conditions tend to be hospitalized for long durations or multiple times over a long period of time, typically have many procedures, and are treated in multiple areas in a hospital. All of these reasons make it very difficult to identify where and when the source may have occurred.
Investigating after the outbreak has begun also makes it challenging, because a negative result from environmental testing doesn’t rule out a source that may have since been eliminated through disinfection.
As Dr. Eric Chow, Chief of Communicable Disease for Public Health – Seattle & King County said,
“Environmental testing for a specific strain of bacteria can be like finding a needle in a haystack, especially because bacteria can be found in places such as sinks or drains. That’s why continued diligence by hospitals in infection control, including hand hygiene is so critical.”
We continue to work with VMMC to provide infection prevention guidance, including re-training staff on hand hygiene.
What’s Public Health’s role in working with hospitals with cases or outbreaks of infections like Klebsiella?
We are responsible for working with healthcare facilities in King County to investigate and respond to reportable cases and outbreaks. This includes the following:
- Support monitoring, identifying and investigation of additional cases and suspected cases
- Attempt to determine whether the cases are healthcare-associated versus community-acquired.
- Facilitate specialized testing when needed through the public health laboratory system
- Identify strategies to decrease risk for further cases
- Provide recommendations based on standardized guidance where available and provide additional guidance as appropriate.