Weighing kids at school has more pros than cons but the reasons may surprise you

By Tim Olds, University of South Australia
A proposal by Global Obesity Centre at Deakin University in Victoria, Australia to measure the height and weight of all Australian school children has understandably generated controversy. Some commentators have labelled it misguided, fearing it could encourage kids to “pursue weight loss at any cost”.
While there are benefits and downsides of measuring kids’ height and weight at school, the pros outweigh the cons.
But some reports have confused the purpose of the scheme, which is intended to generate data to inform obesity research and policy responses, rather than provide feedback on the individual child’s health status.
Let’s start at the beginning at look at the difference between screening and surveillance, and what the Deakin team has proposed.
BMI report cards
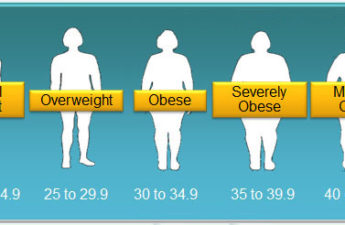
Screening programs weigh kids to identify those who are at risk of health problems associated with their fatness. This is generally based on BMI (body mass index), which measures weight in relation to height. The results of the screening – “BMI report cards” – are sent to parents, and sometimes to the kids and schools as well.
Read more:
Does my BMI look big in this? And does it really matter?
Screening programs are rare in Australia, but are widely used in several US states, notably Arkansas and California.
The logic behind screening is that obesity is a health issue like ADHD or movement disorders, and schools have a duty of care to report these conditions to parents. There is strong evidence that parents are not very good at identifying the weight status of their children.
Screening programs are controversial. In the US, they are generally well-received by parents, who claim to take action if their child is identified as overweight.
But there is growing evidence that these programs are ineffective.
Collecting data for research
The Deakin group is not recommending BMI screening or BMI report cards. They are arguing for a system of surveillance, which is quite different.
Surveillance is the systematic collection and analysis of data on kids’ fatness from a representative sample, or from a census.
For surveillance purposes, neither children, nor the teachers, nor the parents are told the child’s BMI. Children may be identified by coded numbers which are known only to the researchers.

Belinda Pretorius/Shutterstock
Parents can opt out by ticking a box, and no measurement can be made without the verbal assent of the child.
Measurements are done by trained clinicians, in private.
No child, parent or teacher is made aware of any measurement, and any questions about the results are defused by comments such as:
Kids of your age come in all shapes and sizes, and anyway, they change so quickly. If you’re worried, why not ask your mum or dad to measure you?
These procedures are now standard practice in research settings.
Downsides of weigh-ins
The biggest concern is that overweight (or underweight) kids may feel sensitised to weight issues, and may adopt unhealthy weight management practices like purging or extreme dieting.
Read more:
Health Check: should you weigh yourself regularly?
A review of the Arkansas program found that 7% of kids were embarrassed about being weighed at school. It is likely that some kids will be distressed by the procedure.
In one discussion forum, a mum said:
I experienced eating disorders in high school and if I knew there were weigh-ins (even occasionally) it’d send me into a near-constant state of panic and restricting and purging.
Other kids may find the “normalisation” of weighing reassuring.
The Arkansas review found that kids were not more likely to be teased about their weight, or go on diets, or have more concerns about body image after the introduction of the measurement program.
Some people feel that obesity is not a disease, that kids can be healthy at any weight, and that we should be focusing on behaviours such as healthy eating and physical activity, not fatness.
However, there is a strong association between fatness a wide range of diseases, notably diabetes, and pretty powerful genetic and experimental evidence that the relationship is causal.
So what are the benefits?
The main benefit is that BMI surveillance will provide a rich source of accurate data.
At the moment, we only collect data on samples of kids who put up their hands to be measured. As you would expect, fatter kids are less likely to do this, so our data underestimate, and by a pretty large margin, how many kids are overweight or obese.
In one study, an opt-in method estimated obesity prevalence at 10%. The opt-out method estimated 14%.

kwarkot/Shutterstock
Having regular, opt-out, population-level surveys of kids’ height and weight allows us to chart historical trends, geographical distributions, and, if measurements can be linked to de-identified personal data, associations with socioeconomic status, environments, and health outcomes.
All this helps to direct resources where they are needed, and to plan more effective interventions.
Read more:
The real reasons why parents struggle with children’s portion sizes
The potential uses of data of this sort are enormous. Here are two examples.
Some recent studies have linked obesity to air pollution. By looking at the associations between where kids live, their exposure to pollution, and fatness, we can test this theory.
![]() Another recent study in the US found that the entire increase in children’s fatness in the first three years of primary school occurred during the summer holiday period. By weighing kids at the start and end of each school year, we could see if the same thing is happening in Australia.
Another recent study in the US found that the entire increase in children’s fatness in the first three years of primary school occurred during the summer holiday period. By weighing kids at the start and end of each school year, we could see if the same thing is happening in Australia.
Tim Olds, Professor of Health Sciences, University of South Australia
This article was originally published on The Conversation. Read the original article.