By Sabin Russell / Fred Hutch News Service
Cancer patients in rural areas of the United States die of their disease at significantly higher rates than those residing in U.S. cities, and scientists at Fred Hutchinson Cancer Research Center in Seattle are trying to find out why. Now, they have uncovered an important clue.
This week, they and colleagues at SWOG, a network of cancer researchers from 47 states, published evidence that when rural and urban patients receive identical care — as participants do in carefully controlled clinical trials — those alarming differences in survival rates virtually vanish.
“When patients are enrolled in clinical trials, where patients are uniformly assessed, treated and followed under strict, best-practice protocols, there was almost no difference in survival rates between rural and urban cancer patients,” said Dr. Joseph Unger, the Fred Hutch health services researcher and biostatistician who led the study.
This implies that cancer patients in the countryside — about 19 percent of U.S. cancer patients — would likely survive just as long as their city-dwelling counterparts if they routinely had the same access to “guideline care” available in clinical trials, Unger said.
The study is the largest ever conducted comparing cancer survival of patients receiving clinical trial care in rural versus urban areas of the United States. Unger and his SWOG team published their results Aug. 17 in JAMA Network Open, a new online, peer-reviewed journal of the American Medical Association dedicated to releasing research findings as quickly as possible and making those findings “freely available to all readers.”
A surprising finding
A report last year by the Centers for Disease Control and Prevention found that the death rate from cancers in rural counties in the U.S. was 180 per 100,000 persons, compared to 158 per 100,000 in large metropolitan areas during the five-year period, from 2011–2015. The differences in survival rates have in fact long puzzled researchers, who need to consider complex factors such as environmental exposures, behavior, age, race, gender and access to care as possible reasons.

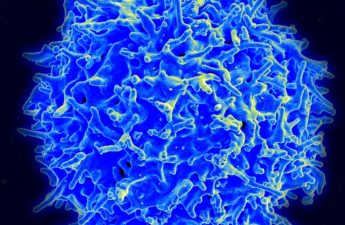
In their search to explain this disparity, Unger and his team scoured records of nearly 37,000 cancer patients enrolled in 44 different SWOG clinical trials that took place across the United States from 1986 through 2012. The trials covered 17 different types of cancer, including acute myeloid leukemia, sarcoma, lymphoma, myeloma, and brain, breast, colorectal, lung, ovarian and prostate cancers.
The result was surprising: for 16 out of 17 cancers, there were no meaningful differences in survival outcomes.
The one exception was a roughly 25 percent higher risk of death for rural patients with a very specific type of breast cancer (estrogen-negative and progesterone-negative).
“We don’t really have a good answer for that one,” Unger said. “It might represent something very particular about delays in treatment administration, or it could be a random finding.”
A proxy for access to best-practice care
The SWOG findings have a strong statistical foundation due to the large number of participants and the wide variety of cancers involved. Because clinical trials require a strict protocol, the researchers could use participation in them as a proxy for having access to guideline-based, best-practice care. When the results showed the survival disadvantage of rural areas disappear, “it suggests that the big deal is access to guideline-based clinical care,” he said.
Unger and his co-authors recognize that a limitation of the study and its analysis is that the results might not be the same in comparisons of urban and rural patients who receive quality care outside of the tightly controlled clinical trial setting. He noted that one of his earlier SWOG studies, published in the Journal of the National Cancer Institute in 2014, found cancer survival outcomes were better among clinical trial patients than for those who received similar care outside of the research setting. However, that apparent advantage for trial participants disappeared after the first year of follow-up care, suggesting similar outcomes over the long term.
Underscoring the need for equity in health care

Dr. Beti Thompson, a Fred Hutch researcher who specializes in barriers to cancer in disadvantaged communities but who was not a part of Unger’s new study, said the work focuses much-needed attention on the availability of adequate care.
“It says what we have been advocating for a long time — if individuals have equal access to care, their survival is also equal,” she said. But she noted that access to care is not standard in many rural areas and it can be difficult to locate, let alone travel to locations providing such care.
Thompson added that equal access to care may not only eliminate rural/urban differences in treatment outcomes, but also health disparities among racial and ethnic minorities.
The National Cancer Institute and The Hope Foundation funded the study.
Sabin Russell is a staff writer at Fred Hutchinson Cancer Research Center. For two decades he covered medical science, global health and health care economics for the San Francisco Chronicle, and wrote extensively about infectious diseases, including HIV/AIDS. He was a Knight Science Journalism Fellow at MIT, and a freelance writer for the New York Times and Health Affairs. Reach him at srussell@fredhutch.org.