From the University of Pittsburgh
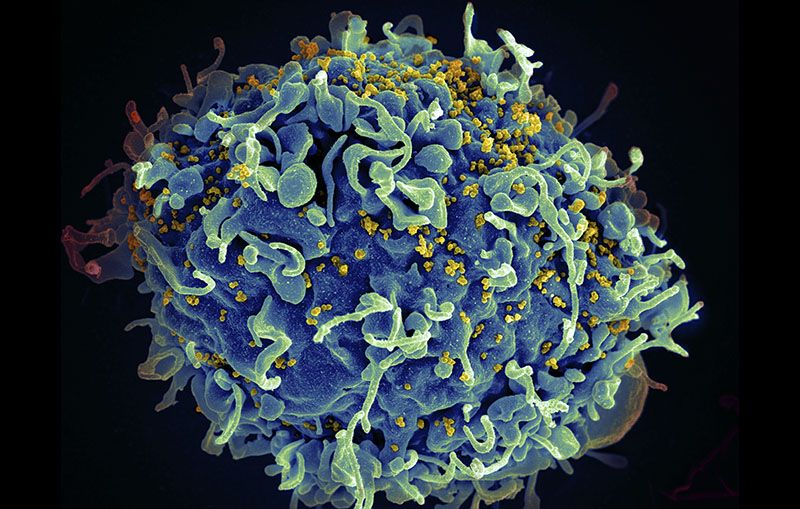
Even after nearly a decade of strict HIV treatment, cells sheltering the virus could be found in the cerebrospinal fluid of half of participants in a national clinical trial of people living with HIV.
Moreover, those participants had a higher likelihood of cognitive deficits than their peers without cells harboring HIV in their spinal fluid, according to an analysis published today in the Journal of Clinical Investigation.
The study, led by scientists at the University of Pittsburgh School of Medicine, Yale University and the University of North Carolina. Anne C. Collier, M.D., director of the UW’s AIDS Clinical Trials Unit at Harborview and a UW professor of Allergy and Infectious Diseases and Medicine, was a co-author on the paper.
The findings may help answer questions about why people with well-controlled HIV still experience problems with memory, concentration and the ability to complete complex tasks. It also points to an important reservoir for the virus in the brain that cannot be overlooked in clinical trials testing a cure.
“I don’t know of a single infectious disease that is easier to treat when it’s in the brain, than when it’s elsewhere in the body,” said senior author John Mellors, M.D., professor and chief of Pitt’s Division of Infectious Diseases. “It is difficult to target infections that lurk in the brain and HIV is probably not an exception to the rule. We have our work cut out for us in the quest for an HIV cure, but knowing is half the battle, so I’m cautiously optimistic.”
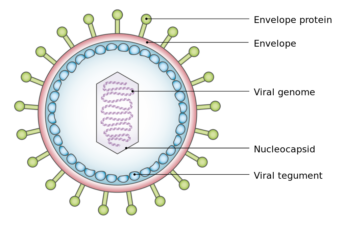
Many people who receive long-term treatment continue to harbor HIV DNA in a few blood cells. These cells can cause a recurrence of active infection when treatment is stopped, so clearing the body of all HIV DNA has been a focus of efforts to develop a cure.
However, the persistence of cells with HIV in the central nervous system–specifically in the cerebrospinal fluid that surrounds the brain and spinal cord–was not well recognized.
With funding from the National Institutes of Health (NIH) AIDS Clinical Trials Group, the research team examined cerebrospinal fluid from 69 people, all of whom had been on anti-HIV therapy for an average of nine years. Very sensitive methods of detecting HIV revealed that almost half of the participants harbored viral DNA in cells found in the cerebrospinal fluid. Of those, 30% met criteria for cognitive impairment, compared with 11% of those who did not have cells with HIV in their cerebrospinal fluid.
The researchers stressed that the presence of these cells did not clearly cause the cognitive impairment and that there could be several explanations for the findings. For instance, it is possible that the level of original infection in the nervous system was higher in the group with the cells harboring HIV or that the development of cognitive problems may have been set in motion early in the HIV infection, before the anti-HIV therapy was started.
Mellors noted that, while treatment is not yet available to clear HIV from cerebrospinal cells, the finding still has potential clinical applications. Awareness of the potential link between HIV infection, even when well-controlled, and cognitive issues can help physicians to track patients who may need additional monitoring.
Co-lead author Serena Spudich, M.D., the Dr. Harry M. Zimmerman and Dr. Nicholas and Viola Spinelli Professor of Neurology at Yale University, noted that future clinical trials will be needed both to establish a reason that a cerebrospinal HIV reservoir would be linked to cognitive decline, and to determine if eliminating this reservoir is possible and if doing so improves neurocognitive function in people living with HIV.