By Michael Ollove, Stateline
A mountain of evidence proves it: Good health translates to better student performance.
Children who have high blood pressure or are obese perform worse academically than others. Children with asthma miss far more school. Students who have healthy diets, who are physically active, who abstain from alcohol and illicit drugs, get better grades.
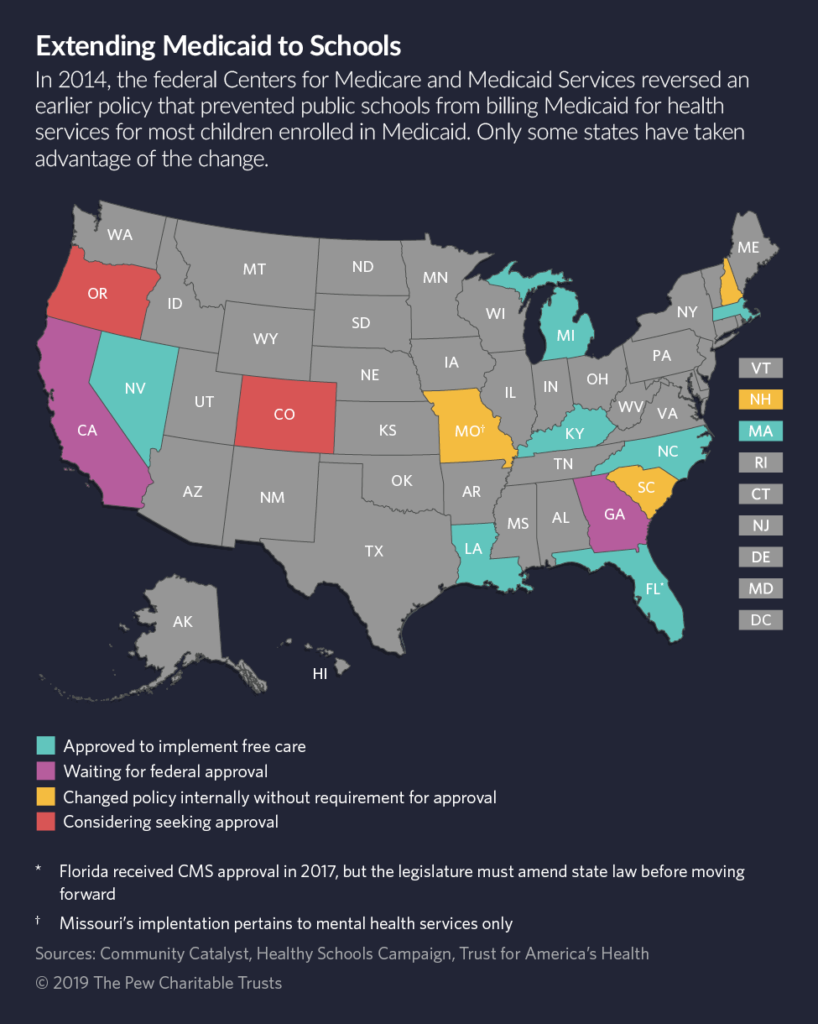
With that in mind, more than a dozen states are finally taking advantage of a five-year-old federal policy change that would make it easier for schools to provide health care to millions of children across the country.
Before the change, the federal government barred school-based clinics and providers from billing Medicaid, the joint state-federal health care program for the poor, for care provided to children on the Medicaid rolls.
The federal government reversed that policy in 2014, but only now are some states taking advantage of the shift. About 45 million children are enrolled in Medicaid.
One possible reason for the delay is that officials at the U.S. Centers for Medicare and Medicaid Services, or CMS, tend to communicate with their counterparts at state Medicaid agencies and health departments, not departments of education.
Now that they can bill Medicaid, more schools will be able to help students manage chronic conditions such as asthma, diabetes and food allergies; offer mental health and addiction treatment; and provide dental, vision, hearing and speech services. Schools that have been providing those services with their own money can now spend it on other things.
“We know kids aren’t getting the health care they need, especially vulnerable populations and children of color,” said Alexandra Mays, executive director of the Healthy Schools Campaign, a Chicago nonprofit that pushed hard for the federal policy change. “Schools are where the children are.”
Florida, Kentucky, Louisiana, Massachusetts, Michigan, Nevada and North Carolina have received permission from CMS to bill Medicaid for health care in schools. California and Georgia are awaiting approvals, and Colorado and Oregon are preparing paperwork.
“We are very excited, and our school districts are excited as well,” said Wayne Lewis, commissioner for the Department of Education in Kentucky, which received CMS approval in November.
Lewis said the Medicaid money will help Kentucky beef up mental health services in schools. A new Kentucky law directs schools to have at least one school counselor for every 250 students.
In Nevada, which received CMS approval in October, officials also want to deploy more mental health professionals to schools to combat an uptick in suicides and to prevent school shootings.
Suicides among young people nearly doubled in Nevada between 2017 and 2018, according to the state’s health department.
“We feel that getting more hands into the schools to help our teachers is a great thing,” said Christy McGill, director of the Office of Safe and Respectful Learning Environment in the state Department of Education.
The federal ban on Medicaid reimbursement was enacted in 1997, when CMS decided that since schools weren’t charging insurers for health care provided to other students, they couldn’t bill Medicaid for the care they provided to children enrolled in Medicaid. It had a severe impact on schools with a lot of students from low-income families. In Chicago, for example, more than 60% of public schoolchildren are enrolled in Medicaid.
“It was just ineptitude,” said Sasha Pudelski, advocacy director at the American Association of School Administrators. “It really wasn’t well thought through.”
The ban allowed schools to bill Medicaid for care provided to students in special education. In 2016, before any state had taken advantage of the 2014 policy change, the federal government spent nearly $4.5 billion on school-based health care for Medicaid-eligible students.
That amounts to less than 1% of federal Medicaid spending, but it is one of the top sources of federal dollars for public schools.
A 2018 survey by the school administrators association found that almost 70% of school districts used the special education Medicaid money to support the salaries of health professionals. That percentage should increase under the broader reimbursement policy.
Georgia officials want to bill Medicaid for school nurses. They estimate federal reimbursements will increase by nearly $49 million, nearly doubling the amount they currently receive ($54 million) for health care for students with special needs.
But some states don’t know how much Medicaid money they will receive.
In Utah, Scott Jones, deputy superintendent for the state board of education, said the final tally will depend on which health services the legislature and the school districts decide to offer.
“We’re looking at tens of thousands of students, if not hundreds of thousands of students, depending on what services we go after,” said Jones, who has held his position for three years but said he became aware of the policy change only a year ago.
In Kentucky, Lewis, the education commissioner, said school districts will decide whether to pursue more Medicaid money.
But some school officials worry that red tape will deter cash-strapped districts: In the school administrators survey, 43% of rural and suburban districts and 37% of urban districts said the required paperwork was difficult.
Under Medicaid, each state must match between 50% and 77% of the federal contribution, depending on its poverty rate. But many states don’t expect to put additional dollars toward health care in schools.
Thomas Stinson, a nurse at Harding High School in St. Paul, Minnesota, and a member of the American Federation of Teachers committee on health policy, said states would be foolish not to tap into the federal money.
“This is a no-brainer,” Stinson said. “All this talk about the need for mental health and to not be on board? It pisses me off.”