Early study of COVID-19 patients shows high mortality rate

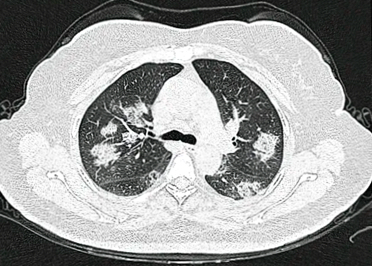
A study of 24 of the most critically ill patients with COVID-19, early on in the pandemic, indicated a high mortality rate, and a prolonged time on respirators for the patients who did survive the virus’ attack.
This study, published March 30 in the New England Journal of Medicine, saw a mortality rate of 50 percent. Most of the patients in the study spent an average of 10 days on a ventilator.
Usually the average time a patient in an Intensive Care Unit (ICU) spends on a ventilator ranges from 3 to 7 days, according to one study.
“In this group, once patients required mechanical ventilation, no one came off within the first week, even younger patients in their 20s,” said Dr. Pavan Bhatraju, a pulmonary and critical care physician with the University of Washington School of Medicine and lead author of the study. All the patients were from the Puget Sound area.
“It is important to remember that the vast majority of patients who are infected with coronavirus do not require ICU care. However, when patients are requiring ICU level of care they are often needing extended respiratory and vasopressor support,” Bhatraju said.
These conclusions were reached by an analysis conducted by UW Medicine pulmonologists. They studied the cases of 24 patients in nine hospitals during the early stages of the pandemic in Washington state, which reported the nation’s first COVID-19 death in late February.
The findings suggested that doctors should not be so quick to rule out coronavirus for patients who present only with a cough. The most common symptoms on hospital admission were shortness of breath and cough, which occurred in 21 (88 percent ) of the patients.
Documented fever was present in 12 (50 percent) patients when they came into the hospital, the report states.
“The research indicated that relying on fever may not be a useful criterion to determine severity of illness and that diagnostic algorithms that require fever for COVID-19 testing may delay diagnosis,” the report stated.
The age range was quite wide for patients who had COVID-19. The youngest patient was 23, while the oldest was 97. The average age of the patients was 64 years. Males were 63 percent of the patients.
“Our findings are consistent with other reports that COVID-19 infection can cause severe illness even in younger patients”, said Bhatraju.
Most of the patients had underlying conditions such as diabetes or kidney problems. All were treated in the ICU of each respective hospital. In the respective ICUs all were confirmed to have the coronavirus and all had contracted the virus through community transmission. The last check in with the patients by study authors was March 23.
The complications and poor outcomes of the patients – three of whom were still in the ICU at the study’s completion – came solely from the coronavirus effects. The survey tested for influenza and other viruses in the blood and sputum of the patients. All came back negative. However, some of the patients were chronically ill before they arrived at area hospitals.
Aside from taking a closer look at minor symptoms, Bhatraju hopes the study helps with resources allocations as hospitals now are looking at a surge of cases in the Puget Sound area around mid-April.
A better characterization of COVID-19 infection in critically ill patients in the United States is important to guide decision making regarding critical care capacity and resource allocation, the study states.
The patients came from Harborview Medical Center, UW Medical Center campuses at Mountlake and Northwest, as well as from Swedish and Virginia Mason Medical Centers.
Dr. Carmen Mikacenic, a pulmonologist with Harborview Medical Center, was senior author on the paper.


