By Christine Vestal, Stateline
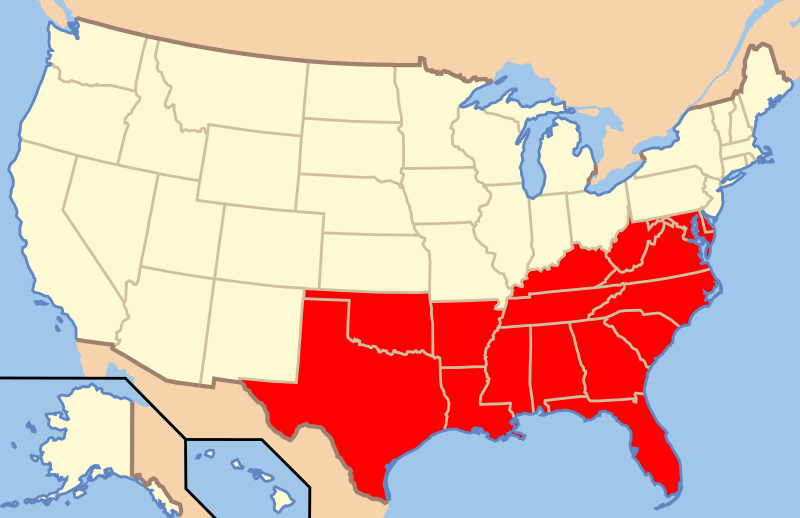
While most of the underlying conditions causing higher rates of COVID-19 infection and death among black and low-income populations can’t be cured overnight, advocates insist political leaders could make a big difference in people’s lives as the region recovers from the crisis.
“The ideological distaste for the Affordable Care Act by many of the South’s political leaders and the Trump administration, has put them at a significant disadvantage to respond to this crisis,” said Joan Alker, executive director of the Georgetown University Center for Children and Families. This crisis could force that to change, she said.
“People in the South don’t just need Medicaid to cover coronavirus treatment, they need it to deal with high rates of chronic disease and to keep rural hospitals afloat. The coronavirus crisis is going to subside, but the economic crisis will be around for a while.”
In general, Southern governors argue that their states can’t afford to expand Medicaid, because they don’t have the money in their limited budgets to pay for even 10% of the bill.
Delayed Shutdowns
The first COVID-19 cases in the country were detected in Seattle in late January, and the outbreak quickly spread throughout the state. New York and other major U.S. cities were next to experience outbreaks.
With the exception of New Orleans, most of the Deep South seemed to be spared initially. Even Atlanta, with one of the largest international airports in the country, did not appear to suffer immediately.
But in late February, two funerals in a small Georgia city 200 miles south of Atlanta set off a chain reaction that quickly overwhelmed local hospitals with COVID-19 patients.
Albany, Georgia, population 75,000, had the state’s first major outbreak, rivaling on a per capita basis those in New York, Seattle and other major cities.
Now similar hotspots are being detected throughout the South. And the virus is seeping into rural communities where many local hospitals are ill-prepared to treat more than a handful of patients at a time.
Lee County, Alabama, on the Georgia border, reported an early outbreak, as did Moss Point, Mississippi, a predominately black town on the state’s Gulf coast, among other small Southern towns.
But even as it became clear that the South would not escape the virus and the Trump administration declared the coronavirus crisis a national emergency March 13, some governors waited weeks to shut down businesses. And in many Southern states, restrictions on businesses are looser than in other parts of the country and messages to the public are reportedly unclear.
Ivey, the Alabama governor, waited until April 4 to shut down certain businesses and order residents to stay at home.
In Georgia, Republican Gov. Brian Kemp issued a limited stay-at-home order April 2, and the next day his administration told local officials who had closed their beaches to reopen them.
In Arkansas, Republican Gov. Asa Hutchinson is still refusing to issue a stay-at-home order. In an interview on PBS NewsHour, he explained that his state was taking a targeted approach to limiting the spread of the virus. Schools and shops — including bars, restaurants, tattoo parlors, barber shops and hair salons — are closed, but otherwise the state is open for business.
“We want to do things that actually work and make a difference,” Hutchinson said. “And our social distancing, our wearing masks is what is working in Arkansas.”
Racial Disparities
Hurricane Katrina and its aftermath laid bare the vulnerability of people living in poverty and highlighted huge health disparities between black and white New Orleanians devastated by the 2005 storm.
The coronavirus crisis is already spotlighting many of those same issues.
In the District of Columbia, black residents make up 45% of the population and nearly 60% of coronavirus deaths.
In Louisiana, African Americans are 32% of the population and more than 70% of coronavirus deaths, as of April 6.
And more than a quarter of black people in the United States are low-wage workers, compared to 16% of whites, according to the Kaiser Family Foundation. This puts them at greater risk of exposure to the virus and income loss.
Before the crisis, 23% of black people had incomes below the federal poverty level, compared to 10% of white people.
Already, far more African Americans are losing their jobs as a result of the crisis compared to the rest of the population, Heiman said, which will make their chances of recovery even more tenuous.
In many Southern states, racial health disparities are stark. In Alabama, where maternal death rates are the third-highest in the nation, black women die at more than twice the rate of white women. And in every other key indicator of overall health, black residents score lower than white residents.
Nationwide, African Americans have higher rates of obesity, heart disease, hypertension, diabetes, asthma and other chronic diseases compared to the rest of the population. Making matters worse in the South are long-standing policies that prevent many African Americans from getting access to health care.
“In Alabama, poverty and poor health are a legacy of decades of racist public policies that have excluded people of color from health care,” said Jim Carnes, policy director of low-income advocacy organization Alabama Arise.
“We’re thinking of COVID as a high-stakes stress test on our system,” he said. “It’s revealing weaknesses and gaps we’ve always known were there. The question is whether the light will be bright enough this time that our officials will be forced to face the reality and address it.”
Stateline, an initiative of The Pew Charitable Trusts.


