Update on Hepatitis A outbreak
Public Health Insider, Public Health – Seattle & King County
April 2020 marks one year since Public Health – Seattle & King County announced the first case of locally-acquired hepatitis A in a person living homeless in King County.
Public Health identified this case in the context of many cities and states across the country experiencing large outbreaks of hepatitis A among people living homeless or who use drugs.
While our community has been fortunate in that to-date we have not experienced an outbreak on the scale seen in other large cities, hepatitis A continues to spread locally, and the rate of infections has increased in 2020.
Hepatitis A cases in King County
While hepatitis A cases in the United States have historically been linked to international travel or contaminated food products, most of the recent infections we’ve seen in King County have been among people who are living homeless or who use drugs.
This population is at higher risk for hepatitis A because they may have limited access to hygiene resources, such as soap and warm water for handwashing.
If an infected person doesn’t wash their hands well, especially after using the toilet, undetectable amounts of the virus can spread from the hands of that person to other objects, surfaces, and foods, and easily infect others.
Since January 1, 2019, a total of 122 King County residents infected with hepatitis A have been reported to Public Health, including one death associated with hepatitis A. Over half (71 people) of these people became sick in the last four months.
For comparison, over the last decade, there have been 5–16 cases of hepatitis A reported in King County residents each year. (You can view more about the number of hepatitis A cases in King County and associated demographics on our hepatitis A dashboard.)
We’ve seen a small reduction in cases of hepatitis A reported to us in April, with a total of 17 confirmed cases this month. There are many potential reasons for this reduction, but we don’t have definitive evidence of the reasons for this drop.
Potential factors include the success of our recent prevention measures, or peripheral impacts due to COVID-19. For example, COVID-19 physical distancing measures might mean fewer opportunities for transmission. Alternatively, fewer people may be seeking medical care for symptoms of hepatitis A infection out of concern about COVID-19 exposure in a medical setting.
Cluster of cases in Seattle’s Ballard neighborhood
Most recently, we’ve seen a cluster of hepatitis A cases among people living homeless in the Ballard neighborhood of Seattle, with a total of 17 cases reported in people living homeless in this area.
Public Health also reported five cases of hepatitis A among people who ate at Ballard restaurant Señor Moose, with meal dates during February 24-26, 2020(see full restaurant outbreak investigation description). None of these five people described any connection to people experiencing homelessness or who use drugs; however, genetic testing of two of the five cases matches the local outbreak strain affecting people experiencing homelessness or who use drugs.
The remaining three cases associated with Señor Moose are pending genetic testing at Centers for Disease Control and Prevention (CDC). Public Health’s investigation of this restaurant cluster is ongoing to help determine how hepatitis A entered the restaurant.
To help address the increase in cases in Ballard, we’ve worked with the City of Seattle’s Navigation Team, a specially trained team responsible for addressing impacts of unmanaged encampments while offering shelter and services to unsheltered individuals.
This includes distributing public health flyers, hygiene kits, and coordinating hepatitis A vaccines. Seattle Parks and Recreation and Seattle Public Utilities installed sanicans with toilets and a handwashing stations in six neighborhoods, including Ballard.
Recently, the City of Seattle and the Seattle Public Library announced the re-opening of restrooms at five library locations including the Ballard Branch, which opened last week.
This reopening is providing additional vital hygiene resources to people living unsheltered in Ballard Commons and other parts of Seattle.
Hepatitis A prevention and response
King County has invested heavily in work to prevent the spread of hepatitis A, particularly to provide hepatitis A vaccines, which is one of the most effective tools to prevent infection and to help mitigate a major outbreak.
Having witnessed the large scale of hepatitis A outbreaks in other states, Public Health began holding free hepatitis A vaccination clinics for people living homeless starting in fall 2017, before we had identified any cases among people living homeless.
We increased this vaccination push in July 2019, when King County allocated $375,000 towards these efforts. And, this year, King County extended this funding, allocating an additional $322,000 for continued hepatitis A vaccinations.
Our vaccination team and community provider partners have continued this work throughout the COVID-19 outbreak and response.
“The vaccination work has been more challenging as our staff are stretched thin responding to COVID-19 and necessary supplies are scarce,” explained Anne Meegan, director for Public Health’s Healthcare for the Homeless Network. “But, I’m so proud of our team for adapting and continuing to provide this necessary preventative service. Hepatitis A is a major threat to people living homeless, who are at higher risk because they have less access to hygiene facilities. This access has been even more limited during the COVID-19 pandemic with the closure of businesses and community services. Vaccinations are key to help protect this community and decrease the risk of large-scale outbreaks like we’ve seen elsewhere in the United States.”
In total, since January 2019, over 2,500 people have been vaccinated by Public Health and Public Health Reserve Corps staff at over 300 free vaccination clinics at shelters, day centers, villages and other sites serving people who are living homeless or using drugs.
In addition, Public Health works closely with community partners, including the Hepatitis Education Project and other community clinics, who have provided nearly 5,000 hepatitis A vaccines in the last year, targeting people at high risk, including those who are unstably housed, people who use drugs, and men who have sex with men.
Public Health has also requested all healthcare emergency departments and primary care clinics in King County to screen patients for the risk factors of a history of homelessness or drug use and offer vaccination on the spot to prevent missed opportunities for protection against hepatitis A infection. Men who have sex with men are also at increased risk for hepatitis A and should be vaccinated.
Hepatitis A in the state and the nation
For more information about Washington state’s hepatitis A outbreak, visit the Washington State Department of Health’s hepatitis A webpage.
Nationally, since the first hepatitis outbreaks were identified in 2016, according to the US Centers for Disease Control and Prevention, 30 states have reported a total of nearly 30,000 cases, including over 300 deaths.
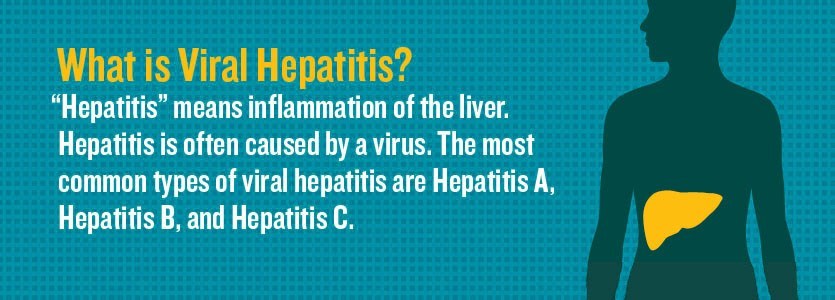
About hepatitis A
Hepatitis A virus infects the liver and can cause illness that ranges from a mild infection with mild or no symptoms to a more severe illness that can last for months.
Hepatitis A virus spreads easily. It gets into the body through the mouth after someone touches an object, food, or drink that is contaminated with the virus.
If an infected person doesn’t wash their hands well, especially after using the toilet, undetectable amounts of the virus can spread from the hands of that person to other objects, surfaces, and foods.
Symptoms of hepatitis A
Common symptoms include tiredness, nausea, vomiting, abdominal pain, loss of appetite, low-grade fever, pale or clay-colored bowel movements and dark urine, joint pain and yellow discoloration of the whites of the eyes and skin (jaundice). Some people get infected with hepatitis A but do not experience all of these symptoms, or even have no symptoms.
People at highest risk for getting hepatitis A
People who are at highest risk are:
- People living homeless, especially those living unsheltered without good access to sanitation, hygiene and handwashing facilities
- People who have direct contact with a person who has hepatitis A, especially those who are living with or caring for a person with hepatitis A infection
- Men who have sex with men
- Illicit drug users (does not have to be injection drugs)
- People with clotting disorders like hemophilia
- International travelers
- People with chronic liver disease, including hepatitis B and hepatitis C are at increased risk for severe infections.
Preventing hepatitis A
Hepatitis A vaccination is the best way to prevent hepatitis A. The shot is safe and effective; anyone who is in the higher risk groups should get the hepatitis A vaccine to protect themselves. In addition, anyone who wants to reduce their risk of hepatitis A infection should get vaccinated.
To get a hepatitis A vaccine, visit your doctor, nurse, or clinic. You can also check www.vaccinefinder.org for pharmacies that offer hepatitis A vaccine. For information about where to get free hepatitis A vaccine for people living homeless: www.kingcounty.gov/hch
Practicing good hand hygiene also plays an important role in preventing the spread of hepatitis A, including thoroughly washing hands after using the bathroom, changing diapers, and before preparing or eating food. People in high risk groups should also avoid sharing food, drinks, drug paraphernalia, and other personal items.
For more information on hepatitis A: