Data from UW Medicine Virology suggests positive test results peaked in late March
Positive results COVID-19 test performed in 10 Washington state counties and in Seattle-area emergency departments began dropping after reaching a peak in late March, an analysis by the UW Medicine Virology lab has found.
The patient samples were from March 1 to April 16. The peak in positive results occurred around March 28 to March 29.
These results suggest that the early and aggressive physical distancing measures enacted in Washington state have influenced the course of the COVID-19 pandemic in Seattle and other parts of the state, the researchers concluded.
The analysis is published today in JAMA, the journal of the American Medical Association.
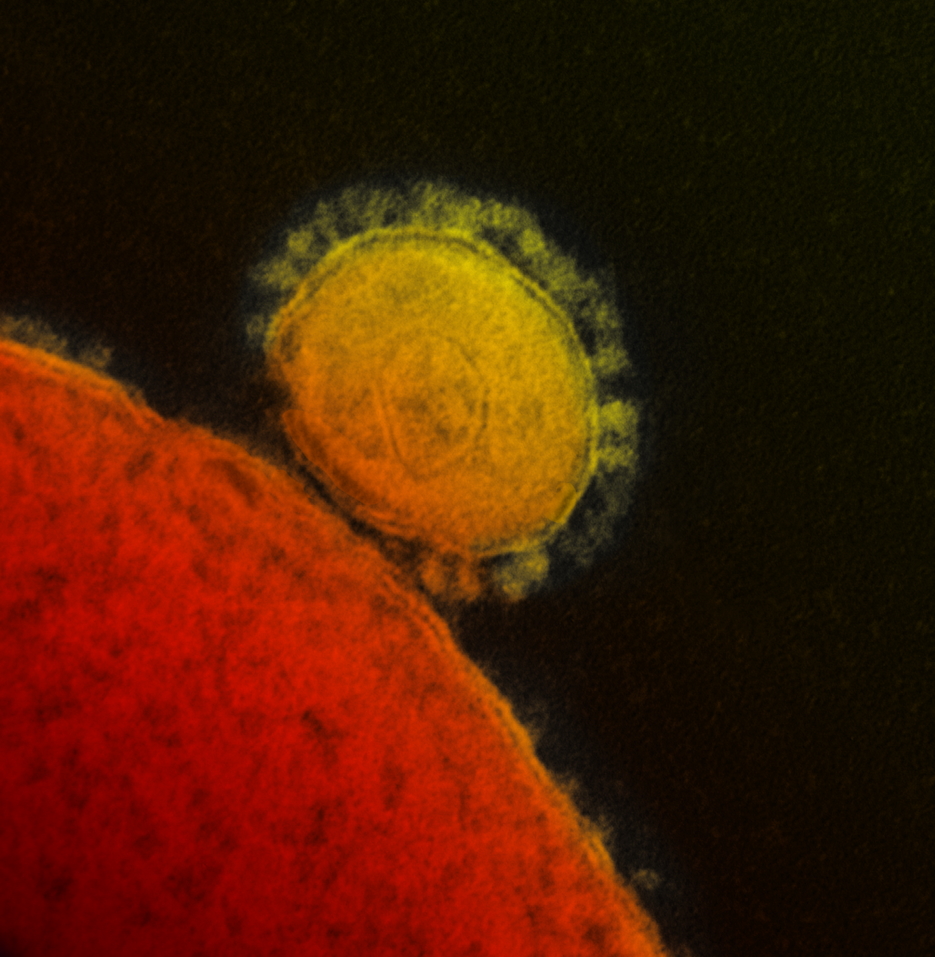
The UW Medicine Virology Lab began testing for Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), the new coronavirus that causes COVID-1, on March 1.
The lab was one of the first, outside of the Centers for Disease Control and Prevention, to test specimens submitted by clinicians for the virus.
Since March 1, the lab has tested samples from more than 95,000 patients in Seattle, other parts of Washington, and from around the United States.
Testing volumes steadily increased for the first half of March and peaked for outpatients around March 12 to March 13. Fewer samples were collected on weekends.
More than 90 percent of the samples came from the UW Medicine healthcare system and outreach clients from different areas in the state of Washington.
The researchers analyzed their data from the testing to look for patterns in the pandemic affecting Seattle and parts of the state at large.
They also wanted to determine the effects of public health mitigation measures, such as physical distancing.
The work was done in collaboration with researchers at Fred Hutchinson Cancer Research Center, which is also in Seattle, ‘
The senior author is Dr. Keith Jerome, professor and head of the Virology Division of the Department of Laboratory Medicine at the University of Washington School of Medicine. He is also a Fred Hutch infectious disease scientist.
There was only limited demographic information available on the patients testing. The researchers found that males had a higher positivity rate than did females.
Positivity rates were higher from patient specimens taken in emergency departments.
While emergency department and outpatient positive rates peaked about the same time, the decline in positive results was more gradual among populations seeking care in emergency departments.
The researchers noted this trajectory of peak and decline seems to align with the local physical distancing guidelines such as the March 16 statewide shutdown of restaurants and bars and social gathering limits, followed by the March 23 “Stay Home, Stay Healthy” order by Washington Gov. Jay Inslee.
Testing criteria did not change significantly over this study period, and remained largely limited to patients showing respiratory and other symptoms suggestive of COVID-19. Testing volume did not increase in the study population due to shortages of sample collection materials.
“The decline in positivity was not due to expanded testing,” Jerome said.
Whether people’s adherence to physical distancing will continue, and how any changes in public behavior, such as the staggered reopening schedule of some public and commercial settings, might alter pandemic infection rates in the coming months remains to be seen.
The Department of Laboratory Medicine at the University of Washington School of Medicine and Fred Hutchinson Cancer Research Center funded this analysis.


