Public Health publishes new COVID-19 key indicators dashboard
Our latest dashboard, Key Indicators of COVID-19 Activity in King County, Washington, provides a snapshot of several useful indicators, or metrics, related to COVID-19 activity in our community and the impact on our health and our hospitals.
We talked to Dr. Jeff Duchin, Health Officer for Public Health – Seattle & King County to learn more about what these indicators mean.
Why are these indicators useful?
JD: The key indicators provide an overview of how we are doing in several important areas: disease activity, testing (specifically, PCR testing), and healthcare system status. The information indicated by these key metrics along with other data and recommendations are provided by Public Health to policy makers when they make decisions about whether current activity restrictions, recommendations and precautions to prevent COVID-19 are adequate, need to be strengthened or might be carefully relaxed.
How do these indicators compare with other data about the COVID-19 outbreak?
JD: In order to understand the impact of the COVID-19 outbreak on King County, Public Health gathers and monitors information from a variety of sources. We display data on public dashboards including a daily outbreak summary, COVID-19 in long term care facilities, emergency department visits, and risk and disparities associated with race, ethnicity, neighborhood, and more.
Do these indicators show us what is happening in the community at the current moment?
JD: No. It’s important to understand that many of the indicators reflect COVID-19 transmission from behaviors and activities that happened 1-3 weeks ago. This is because of the time it takes for someone to become ill after becoming infected (i.e. the incubation period), the time it takes for someone to seek health care and be tested after becoming ill, the time to be hospitalized after becoming ill, and the time to death for severe cases.
Because of the time lag between infection and the outcomes we can observe, if we make changes in our activities and behaviors today that either increase or decrease COVID-19 transmission, we would see the results of those changes (increasing or decreasing numbers of cases) about 2-3 weeks later.
What are the trends in the numbers of reported cases, or “COVID-19 activity,” as it’s called on the dashboard?
JD: This indicator shows the trend in the numbers of new cases for every 100,000 King County residents over time. Our target is to have a downward trend to fewer than 10 new cases for every 100,000 residents over a two-week period, which translates to about 16 cases or fewer per day over 14 days.
The Centers for Disease Control & Prevention (CDC) defines this case level as a “low incidence plateau” for COVID-19 transmission and it suggests our efforts to limit COVID-19 spread are working to prevent the outbreak from growing. The grey bar on the graphical display for this metric shows the current two-week trend. To see more about the number of cases reported each day, also check our Daily Outbreak Summary dashboard.
Is the outbreak growing, shrinking or staying stable?
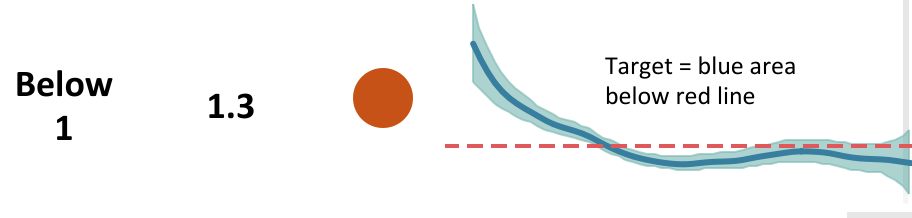
JD: There is an important measure on the dashboard called the effective reproductive number, Re. Re tells us how many other people become infected on average from each person with COVID-19. When Re is under one, each person with COVID-19 spreads the infection to fewer than one other person and the outbreak will shrink. When Re is greater than one, each person with COVID-19 spreads the infection to more than one other person and the outbreak will grow steadily unless additional measures are taken to interrupt spread. The larger the Re, the faster the outbreak grows.
For the reasons explained above (plus a delay needed to update reports used for this calculation), the Re result reflects COVID-19 transmission that occurred about 1-3 weeks ago. The blue area is the range that Re is estimated to fall within and illustrates the uncertainty around the estimate (meaning 95% likelihood that the true result is in that range) with the dark line being the best estimate. Our target is for the Re estimate, including the uncertainty range, to be entirely below one. This measure is provided by the Institute for Disease Modeling, using a model specific for COVID-19 transmission in King County.
There are other metrics for COVID-19 activity that measure risk of hospitalization and death. Is the risk for being hospitalized or death from COVID-19 changing?
JD: These two indicators reflect the direction of the outbreak through two serious health outcomes. When we are effectively limiting COVID-19 spread, the numbers of hospitalizations and deaths fall. Our target is to see these numbers decreasing as much as possible to steady levels that are manageable by the healthcare system.
Testing is an important step in addressing the pandemic so that we know who is getting infected. Are we doing enough testing to detect most cases?
JD: In order to have a reliable measure of the number of COVID-19 cases in the community we need to have testing readily available to people with symptoms. If too few tests are done, many people with the infection will not get diagnosed and reported. The PCR test (not the serology test) is done to diagnose active COVID-19 cases.
Although there is no scientific way to predict exactly how much testing is needed, we use an estimate for our target that is based on the amount of testing done in other countries that have done a good job identifying cases and limiting COVID-19 transmission. This target suggests that for each positive case detected there should be 50 or more tests done.
You mentioned earlier that there can be a delay between when a person starts to feel ill and when that person gets tested. Are we testing quickly enough?
JD: Testing as soon as possible after symptoms develop provides information to infected people so that they can isolate away from others, and for public health contact tracing to start quickly. Rapid testing, isolation of cases and contact tracing are important in order to decrease the spread of COVID-19 in the community.
The ability to test quickly depends on people knowing the symptoms of COVID-19 and getting a test from their healthcare provider or other testing location as soon as they become ill. It also depends on having enough testing available across the county. Our target is for people to be tested within two days of their symptoms starting.
Another set of metrics addressed the healthcare system’s ability to manage COVID-19 cases. How many beds are occupied in our hospitals and how many are filled with COVID-19 cases?
JD: These measures tell us about stress in our healthcare system. When more hospital beds are filled, there are fewer beds, and staff and resources immediately must become available to meet the demand if the number of patients with COVID-19 (or other illnesses) increases. Our target for hospital readiness is to have 80% or fewer hospital beds occupied and less than 10% of beds filled with COVID-19 patients. This is because hospitalized COVID-19 patents are complex and require a high level of care and resources.
What can you say about how individual actions and behaviors affect these measures?
JD: The level of COVID-19 spread and the severity of its impact on our community are directly related to the actions, behaviors and precautions that we take as individuals and in workplaces, businesses and other locations where we gather. It also depends on the ability of our public health system to respond to outbreaks and to rapidly identify cases and their contacts and prevent spread through isolation and quarantine.
It is critical that we all continue to take precautions to limit COVID-19 spread as we increase our necessary activities, especially in workplaces, businesses and other places where people may gather. If we have too many close contacts with others, do not maintain physical distance, and do not take other necessary precautions to prevent COVID-19 spread like good hand hygiene and wearing cloth masks and face coverings in public, we will see cases, hospitalizations and deaths increase.
Not everyone has the opportunity to stay at home to avoid contact with others. For example, essential workers do jobs that we depend on to keep vital services available and that benefit all of us. And some people live in homes that may not have enough space to have their own room if they get sick. To help protect everyone in our community we all should do everything we can to decrease the risk of COVID-19.
So what can do to keep the number of COVD-19 cases as low as possible and stay healthy?
- Maintain physical distancing when out of the home and limit the size and duration of gatherings.
- Wear a cloth mask or face covering in public and when physical distancing is not possible.
- Wash hands frequently or use hand gel disinfectant.
- Clean and disinfect frequently touched surfaces.
- Understand that poorly ventilated, enclosed spaces are higher risk than well-ventilated or outdoor spaces.
- Longer contact with others is higher risk than shorter contact, even when distancing is possible.
- Know the symptoms of COVID-19, stay home at the first sign of illness and contact your healthcare provider to be tested.
- If a close contact or someone in the household has COVID-19, stay home until 14 days have passed from the last exposure to the ill person.
- Avoid contact with ill people.
- All workplaces, businesses and organizations should take required COVID-19 prevention measures and know what to do if illnesses occur.
- People at high-risk for COVID-19 should be especially careful and continue to avoid all nonessential activities and close contact outside of the home.
For more information:
- About signs and symptoms and how to care for yourself and others: https://www.kingcounty.gov/depts/health/covid-19/care.aspx
- About testing: https://www.kingcounty.gov/depts/health/covid-19/care/testing.aspx
- About face coverings and masks: https://www.kingcounty.gov/depts/health/covid-19/care/masks.aspx
- Other COVID-19 resources: https://www.kingcounty.gov/depts/health/covid-19.aspx
Originally published on May 27, 2020.