David J. Peters, Iowa State University
Rural areas seemed immune as the coronavirus spread through cities earlier this year. Few rural cases were reported, and attention focused on the surge of illnesses and deaths in the big metro areas. But that false sense of safety is now falling apart as infection rates explode in rural areas across the country.
Of the top 25 COVID-19 hot spots that popped up in the last two weeks, 18 were in non-metropolitan counties. Arkansas, North Carolina and Texas all set records in mid-June for the number of people entering hospitals for COVID-19. Georgia’s daily reported death toll from COVID-19 was up 35% compared to three weeks earlier.
As a professor of rural sociology, I have been studying the challenges rural America faces in responding to this pandemic to improve how communities prepare and respond.
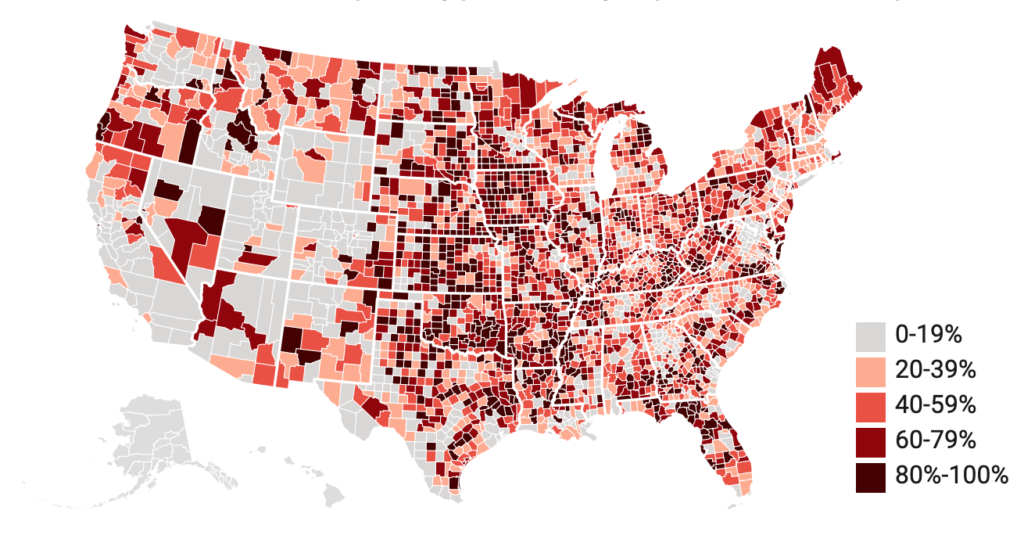
Being able to identify communities that are susceptible to the pandemic before people become ill would allow officials to target public health interventions to slow the spread of the infection and avoid deaths. To do this, I developed a COVID-19 susceptibility scale to assess every county in the Lower 48 states. Susceptibility does not mean an outbreak of COVID-19 will happen, but it means conditions are right for one to occur if the virus is carried in and takes hold.
Why rural populations are at high risk
When you look at the factors that make a population more susceptible to the coronavirus, small communities and rural areas have higher risk factors, as a share of the population, than major cities do.
Rural areas tend to have older populations than the national average, with more chronic health conditions that raise the risk of developing more severe cases of COVID-19. They have fewer health care providers and more uninsured residents, meaning residents often wait longer before seeking medical help. They also tend to be home to large group facilities, such as prisons, meatpacking plants and nursing homes, where the virus can quickly spread to residents and employees can carry it back into the community.
In Iowa, for example, the Tyson plant in Storm Lake drove a 68% increase in confirmed coronavirus cases during the past two weeks. In New Mexico, where new cases rose 42% in the first week of June, about half the new cases were at the rural Otero County Prison. Anderson County, Texas, posted a 10-fold increase in cases when state officials counted infections in five prisons there.
The COVID-19 susceptibility scale uses 11 indicators of the disease based on initial reports from the Centers for Disease Control and Prevention. Those fall into seven distinct risk components: population density; people aged 65 and older; people living in group quarters such as colleges, prisons and military bases; employment in nursing homes; employment in meat processing facilities; people with compromised health; and the prevalence of diabetes. Among people hospitalized with COVID-19, more than 70% have some underlying medical condition, often diabetes or lung or cardiovascular diseases.
Where the high-risk populations are
Looking across the rural-urban continuum, the scale shows that populations in non-metropolitan counties are more susceptible to COVID-19 than in metropolitan ones. That susceptibility increases when going from big cities to rural areas.
Why were big cities overrun with COVID-19 cases? While only 6% of metropolitan counties are at high risk according to my scale, they tend to be our nation’s very large global cities. A small number of COVID-19 cases in densely populated cities can spread rapidly causing numerically large outbreaks. This can quickly overwhelm the health care system, even in large cities. This is what happened in New York City, causing cases to spread across the northeastern U.S.
About one-third of the most rural counties have susceptibility scores in the 80th percentile or higher, as do 29% of semi-rural counties and 19% of micropolitan counties, those with a city of 50,000 people or less. A map of these susceptibility scores shows high-risk communities are concentrated in the Great Plains, Midwest, around the Great Lakes and in some parts of the South.
Some counties are at high risk on just one factor, but have low overall susceptibility. Apache County in northeast Arizona, home to the Navajo Nation, is one example. High rates of diabetes mortality make this group highly susceptible to COVID-19. However, the lower percentage of senior citizens and other risk factors lowers the overall score.
In analyzing the data, some trends stand out.
- Rural counties are primarily susceptible due to their large senior populations. COVID-19 outbreaks are likely to originate in care facilities for the elderly, posing risks for residents and workers alike.
- In semi-rural places, institutions like prisons and military bases add to the risk, as do high numbers of residents who are older or whose health is already compromised.
- Micropolitans are at above average susceptibility due to residents’ health issues, large numbers of meat processing plant workers and care facilities. Semi-rural and micropolitan counties typically provide employment and social services for a region, likely attracting higher-risk populations.
- By contrast, the populations of metropolitan counties have lower susceptibility, though the largest ones face a risk of community spread of the virus because of their high population densities. Cities have lower percentages of older residents and people living in institutional settings. However, a small number of cases in densely populated cities can trigger large outbreaks, driving national cases and deaths.
Researchers at Princeton came to similar conclusions about the high susceptibility of rural counties in a study published June 16 that modeled the impact if 20% of the population in every U.S. county became infected.
Tailoring responses to a pandemic
By knowing how populations are susceptible to severe outbreaks, communities can tailor their responses.
In large metropolitan cities, susceptibility is clearly driven by high population densities, making business closures and shelter-in-place orders essential to slow community spread of COVID-19.
But since rural areas are more sparsely populated, general shelter-in-place orders may be less effective. Instead, rural and micropolitan communities will need to isolate members of specific vulnerable populations quickly. This includes people in poor health, older residents, people living in institutional settings and workers in large meat processing facilities.
To accomplish this, local agencies and providers will need to provide essential services, including food and health care. In many areas, the monumental task of providing these services to a dispersed population will require volunteers and civic groups.
Lack of health care and social services makes rural communities particularly vulnerable. Any state or national response will be hindered by logistical barriers to deploying health providers and supplies over a large geographic area. Limited broadband access means health planners cannot rely solely on telemedicine to fill the gaps in rural areas.
Communities may also see social issues surface. In micropolitan and small metro communities, susceptibility is linked to large meat packing plants whose workforces are predominately Hispanic. Outbreaks may lead to people being treated as coronavirus carriers based solely on their ethnicity and may worsen the marginalization of people based on race.
Different communities have different vulnerabilities to COVID-19, requiring distinctly different strategies to respond effectively to the pandemic across the rural-urban continuum. Such strategies should be developed now to prepare for the next COVID-19 wave.
This story was updated to correct the first link to the susceptibility scale study.
[You need to understand the coronavirus pandemic, and we can help. Read The Conversation’s newsletter.]
David J. Peters, Associate Professor of Rural Sociology, Iowa State University
This article is republished from The Conversation under a Creative Commons license. Read the original article.