PREVENTION IS KEY FOR CONTAINING COVID-19 – HOW CASE INVESTIGATION PLAYS A ROLE
Sharon Bogan, Public Health – Seattle & King County
COVID-19 will be with us for a long time, and we don’t know when we will have a vaccine. That means we need to change the ways we interact with those around us.
The risk of COVID-19 has not decreased. In fact, now that we are interacting with people more, our risk has increased. As long as we are around other people, we won’t be able to eliminate our risk.
But we can reduce the risk if we maintain six-feet distance, wear face coverings when we leave home, avoid prolonged close contact with others, and wash hands frequently.
Paying attention to ventilation is important: outdoors and well-ventilated spaces are lower risk. If we develop symptoms or have been in contact with someone who has tested positive, we should isolate from others and get tested right away.
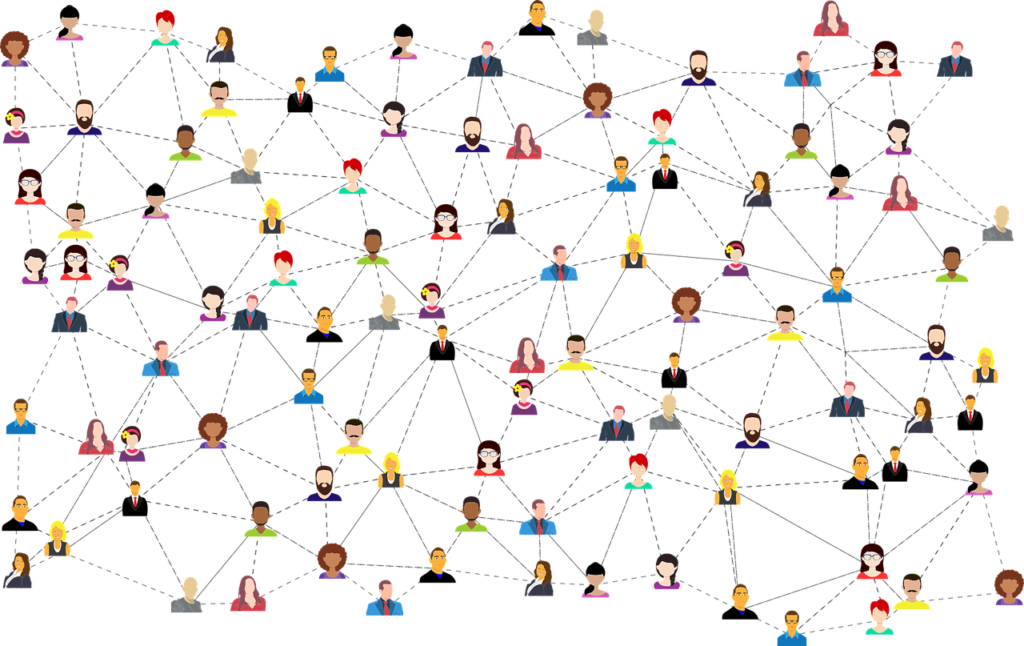
That’s where case investigation and contact tracing come in. Contact tracing involves talking to people who have tested positive for COVID-19 (cases) and identifying the people they have been near and could have potentially infected (contacts).
Public Health investigators talk with these contacts to help them take the steps they need to protect themselves and others. This includes helping people get tested for COVID-19 and ensuring people can quarantine so that they will not infect anyone else.
This may mean providing a safe place to stay away from vulnerable family members until they are recovered, or providing help by delivering food, medication or other needs to the home. Contact tracing is one way that we can interrupt the spread of disease.
Test positive? Becoming a COVID-19 case
For anyone who tests positive for COVID-19, Public Health will use our case and contact investigation teams to help prevent the disease from spreading.
Public Health has been doing intensive case and contact investigations in long-term care facilities and homeless shelters ever since the local outbreak started in late February.
Those locations remain a special focus because the residents and workers are so vulnerable to the illness. Since April, Public Health has been building an approach for case and contact investigation for COVID-19 cases in the community.
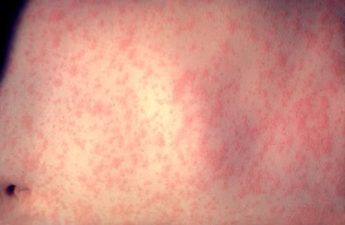
Methods of contact tracing are tried and true, as they are used for other disease investigations – from tuberculosis to HIV, to measles and hepatitis. But case investigation and contact tracing for COVID-19 needs to adapt to the fact that this illness spreads most effectively in the two days before symptoms develop and shortly afterwards, which means staff need to be able to find out about cases very quickly in order to interrupt the chain of transmission.
We are also faced with very large numbers of cases; the scale of the COVID-19 contact tracing effort is unprecedented, at least in modern U.S. history.
Part one is the Case Investigation
Positive test results are reported to the Washington State Department of Health, and then shared with Public Health- Seattle & King County. Each person who tests positive is a COVID-19 “case.”
One of the 22 Public Health investigators (and the numbers are increasing weekly) reaches out to each case by phone for a detailed interview. The more people we can reach, the better chances we have of connecting with their close contacts.
The team asks questions including age, gender-assigned-at-birth, racial identity, the course of the disease so far, and all possible sources of exposure. The interview also focuses on other people who may have been exposed to find out who was in “close contact” with the person during the time when they may have been infectious. This might be people at home, at work, or in the community. A close contact is someone a case has spent 15 minutes or more face-to-face within the two days before they became ill until they are isolated.
Contact tracing information is strictly confidential. Public Health never shares the information collected through contact tracing with other government or private agencies. It is protected health information.
Public Health discusses the medical situation with the individual, provides information about how to safely isolate at home, and links them to care if needed. Each person is offered help so they can successfully remain in isolation and prevent transmission to others.
Part two is the Contact Investigation
Anyone who was identified as being in close contact is now considered a “contact.” At present in King County, each interviewed case has approximately 3.8 contacts. The number of close contacts a person has depends on what type of activities they do and their household size. A Public Health investigator then uses the phone (and other means if available) to reach each of those contacts.
Public Health notifies the close contacts of their potential exposure and refers them to get tested, even if don’t have symptoms.
For the next two weeks, the contact needs to self-quarantine. Public Health is in the process of setting up a system through which a case investigator will call or text each contact daily to monitor how they are doing medically, if they are staying in quarantine, and to see if they need anything like groceries to help them stay at home.
Public Health recognizes the pandemic’s disproportionate impact on some racial and ethnic communities. To help support people from those communities, the team has been hiring investigators from different communities and who are bilingual.
Some key numbers
- Public Health investigates about 200 cases a week. The remainder are investigated by Washington State Department of Health. The proportion and numbers of cases changes depending on how many cases there are in King County each week.
- Public Health has successfully interviewed between 80% and 90% of cases.
- Most cases and contacts are contacted with 24 to 48 hours of Public Health being assigned the case.
“People can be contagious with COVID-19 without showing symptoms. By interviewing people once they are positive and identifying their close contacts, we have the potential to reach people who may have been exposed, but who are not yet showing symptoms,” said Dr. Matthew Golden, who helps lead Public Health’s case investigation team.
“Public Health investigators help people with COVID-19 and the people they have been in contact with get the testing, medical and other services they need. By doing this, we can help prevent further transmission of COVID-19 and protect our community. Our team is working with the Washington State Department of Health, medical providers and community collaborators to rapidly implement a contact tracing system that reaches everyone with COVID-19 and all of their contacts. We are encouraged by the community’s response to this effort and encourage anyone who has symptoms that they think might be from COVID-19 to get tested.”