Lauren Hughes, University of Colorado Anschutz Medical Campus and Jennifer Bacani McKenney, University of Kansas
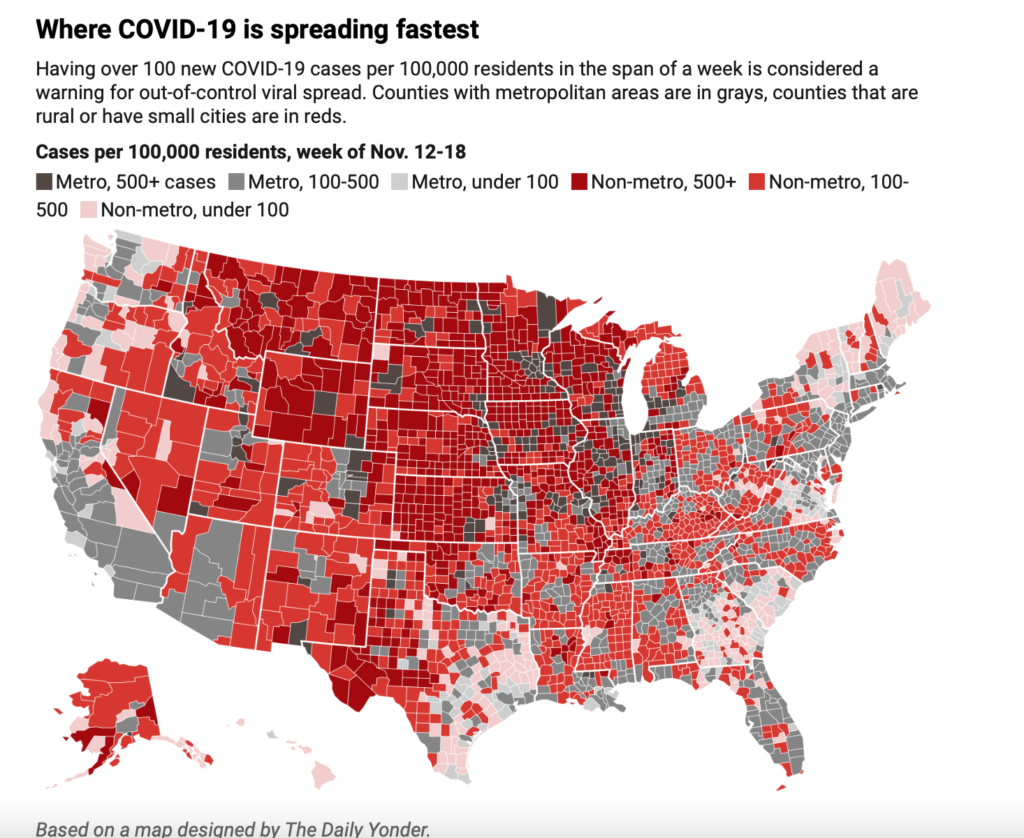
It’s difficult to put into words how hard COVID-19 is hitting rural America’s hospitals. North Dakota has so many cases, it’s allowing asymptomatic COVID-19-positive nurses to continue caring for patients to keep the hospitals staffed. Iowa and South Dakota have teetered on the edge of running out of hospital capacity.
Yet in many communities, the initial cooperation and goodwill seen early in the pandemic have given way to COVID-19 fatigue and anger, making it hard to implement and enforce public health measures, like wearing face masks, that can reduce the disease’s spread.
Rural health care systems entered the pandemic in already precarious financial positions. Over the years, shifting demographics, declining revenue and increasing operating expenses have made it harder for rural hospitals to stay in business. The pandemic has made it even more difficult. In mid-March, most rural hospitals halted elective procedures to slow the spread of the virus, cutting their revenue further, and many have faced price gouging for supplies given extreme shortages.
I work with rural doctors and hospital administrators across the country as a researcher, and I see the stress they’re under from the pandemic. Here is what two of them – Konnie Martin, chief executive officer at San Luis Valley Health in Alamosa, Colorado, and Dr. Jennifer Bacani McKenney, who practices family medicine in Fredonia, Kansas – are facing. Their experiences reflect what others are going through and how rural communities are innovating under extraordinary pressure.
I’ll let them explain in their own words.
Konnie Martin, Alamosa, Colorado
COVID-19 fatigue is real. It’s wearing on people. Everyone wishes we were past this. I read the other day about health care workers being the “keeper of fears.” During COVID-19, patients have disproportionately placed their fears on clinicians, many of whom experience the same fears themselves. I focus on building resilience, but it’s hard.
My hospital currently has seven patients with COVID-19 and can make room for as many as 12. Back in the spring, we converted a visiting specialist center into a temporary respiratory clinic to keep potentially infectious patients separate and reduce pressure on our emergency department.
It’s all about making sure we have enough staff and hospital capacity.
There isn’t any hospital that isn’t under siege, which means that getting patients to the right level of care can be a challenge. In the past few days, we have accepted three transfers from facilities that are on the front range. We’ve never had to do this before. With six ICU beds and 10 ventilators, we are trying to help others.

Influenza hasn’t arrived yet in our community, and I worry about when it comes. We have nearly 40 staff out right now on isolation or quarantine, a staggering number for a small facility. We are having to shift staffing coverage in half-day increments to keep up.
We are not at a point where we are even contemplating bringing COVID-19-positive staff back to work, like the governor of North Dakota suggested. I hope we never get there. We are, however, considering high-risk versus low-risk exposures. If a clinician is exposed to COVID-19 during an aerosolizing medical procedure, that’s high risk. If a clinician is exposed in a classroom of 50 people who were all socially distanced and wearing masks, that’s low risk. If we face critical workforce needs, we may bring back health care workers that have had low-risk exposures.
We have gained a lot of knowledge this year, and we all feel wiser now, but definitely older, too.
Dr. Jennifer Bacani McKenney, Fredonia, Kansas
We chose to live in a rural community because we look out for one another. Our one grocery store will deliver to your home. Our sheriff’s department will drive medications outside of city limits. If we could return to our rural values of caring for and protecting one another we would be in a better position. Somewhere along the way, these values took a back seat to politics and fear.
Wilson County, where I practice in Southeast Kansas, didn’t see its first COVID-19 case until April 15. By August, you could still count the number of cases on two hands. But by mid-November, the total was over 215 cases in a county with a population of about 8,500 – meaning about one out of every 40 residents has been infected.
Our 25-bed critical-access hospital doesn’t have dedicated ICU beds, and it has only two ventilators. Emergency department calls are split among the five physicians in Fredonia. In addition to dealing with COVID-19 cases, we’re managing every other illness and injury that walks through the door, including strokes, heart attacks, traumatic injuries and rattlesnake bites.
We have sectioned off a hallway of rooms for suspected COVID-19 cases. Without an ICU, however, we have to rely on other hospitals. Recently, my partner had to transfer a patient who had a gastrointestinal bleed. She had to call 11 different hospitals to find one that could take the patient.
I feel lucky to have on-site testing in the hospital lab. But like many of my rural peers, getting enough face masks and other personal protective equipment early on was tough.

The community is tired, frustrated and stubborn. Politicians talk about relying on personal responsibility to end the pandemic, but I don’t see a majority of people wearing masks in public spaces despite pleas from health professionals. Some people are scared. Others act as if COVID-19 doesn’t exist.
Politics is making things harder. I have been Wilson County’s health officer for the past eight years. This year, county commissioners gained more control over COVID-19 health decisions.
When I proposed a mask mandate early in the pandemic, one county commissioner argued it would violate his rights. Another commissioner balked at one of my reports, saying I had no right to tell schools how to evaluate kids before they can return to sports, despite the health risks.
I recently proposed a new mask mandate given our rising numbers. I explained that masks would not only save lives, they would help businesses stay open and keep employees at work. The commissioners voted it down 3-0.
Preparing for the next pandemic
We live in an interconnected world where commerce and people cross state and national borders, and with that comes the risk of new diseases. America will face another pandemic in the future.
Rural health care delivery systems can leverage lessons from COVID-19 to prepare. Among other things, their emergency preparedness “tabletop exercises” can include planning for infectious disease outbreaks, in addition to fire and floods; mass casualty incidents; and chemical spills.
They can permanently diversify supply chain options from other industries, such as construction and agriculture, to help ensure access to needed supplies. To avoid staff and supply shortages, they can create regional rural health care networks for swapping staff, conducting testing and acquiring supplies.
Meanwhile, rural doctors and health care administrators are being as flexible and resourceful as they can in the face of adversity.
[Understand new developments in science, health and technology, each week. Subscribe to The Conversation’s science newsletter.]
Lauren Hughes, Physician, Associate Professor of Family Medicine, University of Colorado Anschutz Medical Campus and Jennifer Bacani McKenney, Family Physician, Assistant Dean for Rural Health at the University of Kansas Medical Center, University of Kansas
This article is republished from The Conversation under a Creative Commons license. Read the original article.


