By Christine Jewett, KHN
A prominent group of academics is pressing the Biden administration to move faster and take stronger action to protect high-risk workers from airborne exposure to the coronavirus, urging enforceable standards to help safeguard risky workplaces including health care, food processing and prisons.
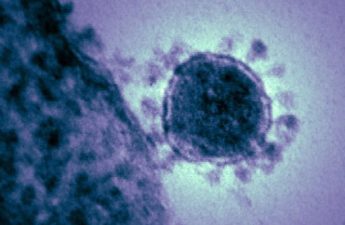
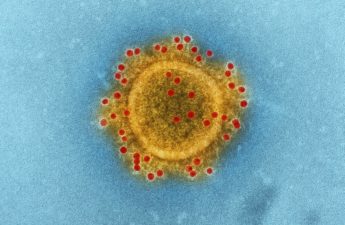
The researchers say that even though the Centers for Disease Control and Prevention has acknowledged the virus can spread through tiny airborne particles, it needs to take “strong immediate” action to update its guidance to reduce the risk.
“This is the opportunity now,” said David Michaels, a professor at George Washington University and former director of the Occupational Safety and Health Administration.
Changes to help drive down the spread of the virus could include broader use of N95 masks in workplaces as well as better ventilation, according to a letter sent Monday to the CDC.
High-profile signers include Rick Bright, who was dismissed from the Trump administration after pushing for more careful attention to science; Michael Osterholm, an adviser to the Biden transition team; and Virginia Tech aerosol scientist Linsey Marr.
Current CDC guidelines reflect the initial supply chain crisis the country faced, which to a large degree has eased, the letter says. They also fail to acknowledge months of research that showed the heightened risks faced by essential workers in several industries.
The letter criticizes current guidelines that say that those outside health care should not get N95 masks, and that even within health care those masks should be reserved for workers doing “aerosol-generating” procedures like intubations.
Yet, since those guidelines were written, research has shown that deadly outbreaks have occurred in meatpacking plants and prisons, with aerosol spread believed to be at play. And within health care, researchers discovered that “front door” staff members like paramedics and those in emergency rooms faced the highest infection risks.
“It really bothers me that health care workers and essential workers who need this extra level of protection have gone this long with a crisis standard of care and without appropriate … respiratory protection,” Bright said in an interview.
Even more recent research that painstakingly examined a September covid-19 outbreak in a Boston hospital with “mature” infection-control practices showed that health technicians caught the virus from a patient while wearing surgical masks and face shields — common personal protective equipment for health workers caring for covid patients. The finding spurred the authors to suggest broader use of N95s throughout hospitals.
KHN and The Guardian have been writing about hundreds of more than 3,400 health care workers who died of covid for the Lost on the Frontline project. Families of many workers have expressed concern about PPE in at least 100 cases, and many others were not aware of what a loved one was wearing. Worker complaints to government officials about protective gear, one story in the series found, preceded a worker’s death in dozens of cases.
Jane Thomason, lead industrial hygienist for National Nurses United, who was not involved with the letter, applauded its contents and said it reflected many of the concerns of nurses the past year.
To add to the list of concerns, Thomason said the CDC guidelines fail to reflect research showing that pre-symptomatic and asymptomatic spread of the virus is common.
Current guidance to hospitals that they screen only patients with covid-like symptoms means that many with the virus slip through and are placed under the care of workers with suboptimal PPE. Thomason said solutions would include universal patient testing and providing the N95 as the minimum respiratory protection in a hospital.
“The crisis standards the CDC created essentially serve as a menu for employers to race to the bottom,” she said. “I think it’s appalling that these are still the same issues a year in.”
The CDC did not respond Tuesday evening. CDC Director Dr. Rochelle Walensky has already announced a thorough review of the agency’s guidelines, based on “the best available evidence,” the letter notes.
Those guidelines will set a standard that workplace safety regulators can enforce, said Lisa Brosseau, a University of Minnesota aerosol scientist who signed the letter. She said CDC acknowledgment of the need to protect workers from inhaling the virus will give OSHA more clout to keep workers safe.
Dr. Donald Milton, a professor of environmental health at the University of Maryland School of Medicine who signed the letter, said now is the time to see how low we can drive virus levels — so we don’t have to shut the nation down again if there’s another pandemic.
“There needs to be a commitment to figuring it out and doing what needs to be done so we never have to do this again,” he said.