By Michael Ollove, Stateline

Democrats in Congress plan to use the $1.9 trillion COVID-19 relief bill to advance President Joe Biden’s campaign promises to make affordable health care available to more Americans, reversing the Trump-era decline in the number of people with health insurance.
They propose to increase federal subsidies to help people buy private health insurance plans and to make those subsidies available to more people.
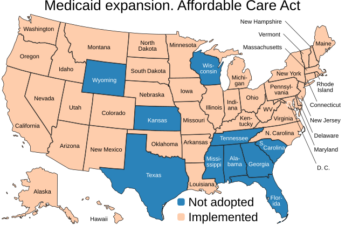
They want to offer new incentives to entice the 12 states that have not yet expanded Medicaid under the Affordable Care Act to do so.
And they want the federal government to temporarily pick up health insurance costs for those who have lost their jobs and their employer-sponsored coverage during the pandemic.
Expanding Medicaid, the more generous subsidies and the other changes related to private insurance could increase the number of Americans enrolled in health insurance by at least 5.3 million, according to various analyses, including one by the Congressional Budget Office and another by the Kaiser Family Foundation.
The progressive, Washington-based research organization, the Center on Budget and Policy Priorities, estimates that under the proposal, if all remaining states expanded Medicaid, they would receive nearly $22.8 billion in additional federal funding over two years. The House Joint Committee on Taxation estimates that more generous subsidies and other changes affecting private insurance would cost the federal government $45.6 billion over two years.
“It took my breath away when I saw the proposals,” said Judy Roitman, director of the Tennessee Health Care Campaign, which advocates for affordable health care in the Volunteer State.STATELINE STORY December 9, 2020Trump Takes a Final Shot at Obamacare Exchanges
Democrats are pursuing other measures in the COVID-19 relief package as well, including extending the time new mothers on Medicaid can receive benefits after giving birth, and enrolling soon-to-be released incarcerated people in Medicaid.
Additionally, the Biden administration last week announced it was rescinding permissionsthe Trump administration had given states to require Medicaid enrollees to work in order to receive benefits. The Trump administration cleared 13 states to impose work requirements, but courts have halted them. A case involving work requirements is now before the U.S. Supreme Court.
The COVID-19 package is likely to land on Biden’s desk. Democrats control both houses of Congress, and in the Senate, they are likely to use a legislative mechanism for budgetary matters that will allow them to sidestep a Republican filibuster, meaning they only need a simple majority. The health measures could be modified before final House approval or after the legislation reaches the Senate.
The package of health measures is in line with Biden’s campaign pledge not to replace the Affordable Care Act—arguably the signature piece of legislation signed by President Barack Obama—but to extend its reach.
“This is a down payment on the type of more comprehensive reform that [Biden] talked about during the campaign,” said Linda Blumberg, an expert in health policy and insurance at the Urban Institute, a nonpartisan think tank in Washington, D.C.
The increased health care subsidies and other changes related to private health insurance could increase the number of Americans with health insurance by 1.3 million, according to a Congressional Budget Office analysis.
Republicans have so far balked at the $1.9 trillion price of Biden’s COVID-19 package. A group of 10 GOP senators countered with a proposal to spend roughly a third of that amount.
More Generous Subsidies
The subsidies, or premium tax credits, included in the ACA are designed to help low- and middle-income Americans purchase individual (as distinct from employer or union-sponsored) health insurance plans on the health insurance exchanges created by the law.
Under current law, there are no subsidies for people whose incomes fall below 100% of the federal poverty line or whose incomes exceed 400% of the poverty line. Under the proposed changes, no one making less than 150% of the poverty line would have to contribute anything for health insurance bought on an exchange.
In addition, some people making less than 100% of poverty or more than 400% of poverty could receive the subsidies. And low- and middle-income people who are already eligible for help would get more of it.
The subsidy changes would be in effect for two years, although advocates hope they would eventually be made permanent.
“This is a safety net for everyone,” said Frederick Isasi, executive director of Families USA, which advocates for affordable health care. “It says that no matter who you are or where you live, if you haven’t got employer health insurance you should not have to pay more than 8.5% of income for a good plan.”
But Edmund F. Haislmaier, a senior health policy analyst with the conservative think tank the Heritage Foundation, isn’t convinced the extra money will help many people at the lower end of the income scale. At those incomes, he said, “those not buying insurance are not doing it for lack of a subsidy.” There are places where they can get health care for free if they need it and aren’t motivated to purchase it, he said.STATELINE STORY November 24, 2020Biden Likely to Help States Increase Health Care Access
Another related provision of the House bill would treat people who have lost their jobs and are receiving unemployment insurance as if they are at the lower part of the income scale, making them eligible to receive the largest subsidies.
Biden already has taken two other actions to spur enrollment in the health plans. This week he opened the federal health exchange, used by the 36 states that don’t operate their own, for an extra three months. The Trump administration had refused entreaties from some governors and health care providers to open the exchange beyond six weeks in the fall to ensure more Americans had access to health insurance during the pandemic.
The Biden administration also announced it would spend $50 million to advertise the exchange and provide counselors to help people choose and enroll in plans.
The House’s COVID-19-relief package also would fully subsidize COBRA health insurancethrough September for workers who lost their employer-sponsored health insurance during the pandemic. Under COBRA, some people who lose their jobs can stay on their former employer’s insurance plan if they pay the premiums themselves.
Enticing States
Biden and congressional Democrats also want to entice the 12 states that haven’t yet expanded Medicaid to do so. That could bring an additional 4 million people into Medicaid, according to the Kaiser Family Foundation.
Medicaid is jointly financed by the states and the federal government, with the federal government chipping in between 50% to nearly 78% for traditional Medicaid programs, depending on a state’s average per capita income compared to the national average. The federal government pays 90% of the costs for Medicaid expansion populations in the states that have taken up the option.
The House bill proposes to offer each nonexpansion state a 5-percentage point boost in their traditional program matching rate for two years if they agreed to join the Medicaid expansion.
So, for example, the federal government now accounts for 66.1% of the Medicaid spending for the state of Tennessee, one of the nonexpansion states. Under the bill’s proposal, the federal share would climb to 71.1% for two years. That would amount to an additional $1.7 billion over two years in federal Medicaid funding, according to the Center on Budget and Policy Priorities.
Whether that sum will attract states that have refused other inducements over the years is unclear. “I can say that the governor has no plans to expand Medicaid,” said Laine Arnold, a spokesperson for Tennessee Republican Gov. Bill Lee.
Still, the number of states opting for expansion has steadily grown over the years—in some states via ballot measure instead of legislative action. And even without the additional enticement, Republican elected officials in some red states, such as Texas and Alabama, recently have signaled a willingness to consider expansion.
In Kansas, Democratic Gov. Laura Kelly this month launched a legislative effort to expand Medicaid there. And health care advocates in Florida, Mississippi and South Dakota are exploring launching ballot initiatives in the wake of successes elsewhere, including deeply conservative Nebraska and Oklahoma.
The other proposed Medicaid changes also would be significant. One would enable states to keep new mothers on Medicaid for a year after delivery instead of the current required 60 days. That provision would pertain only to nonexpansion states, because low-income women in expansion states are already eligible for Medicaid.
Another provision would permit states to enroll soon-to-be-released incarcerated people into Medicaid to ensure they have a smooth handoff to health care services once they are free. The incarcerated population is less healthy than the general public and experiences an especially high death rate immediately after leaving prison, which is why advocates say it is important that they have immediate access to health care after release.
Both of those steps, said Michael Miller, director of policy at Community Catalyst, a Boston-based organization that advocates for expanding health care access, would help address health disparities for people of color.
While much of the impetus for the enrollment-oriented proposals from Biden and Democrats arises from the pandemic, many health access advocates are hoping the changes become permanent.
“The idea that we can do more on the enrollment side has a life beyond the moment and is maybe more enduring,” said Miller.