By Christine Vestal, Stateline
Last year was a nightmare for nearly everyone in health care. But for school nurses, 2021 has been worse.
Since school doors opened this fall, school nurses have been working nonstop on COVID-19 contact tracing and quarantines. In most places, they’ve had to abandon many of their regular duties and add brutal weekend and evening hours to their schedules.
Janis Hogan, a 22-year veteran of school nursing, is among them. Her job at Camden Hills Regional High School in Rockport, Maine, has been reduced to COVID-19 contact tracing all day every day, she told Stateline.
Missing are the one-on-one interactions with kids that she said are invaluable to their physical and mental well-being and academic achievement—and the most rewarding part of her job.
The Biden administration promised in May that help for school nurses was on the way. As part of a $7.6 billion fund created under the American Rescue Plan Act to reinforce the public health workforce, $500 million was set aside to bolster school-based health services.
But a severe nationwide shortage of registered nurses and the unrelenting need for nurses in hospitals overrun with COVID-19 cases mean that much of the new federal money likely will be spent on support for school nurses such as training, scholarships, administrative staff and other contract services—not on fresh troops.
“The goal of the federal relief money was to invest in ways that would address the immediate and long-term impact of the pandemic on kids in schools and to help schools maintain a safe and healthy environment,” said Linda Mendonça, president of the National Association of School Nurses.
Hiring more school nurses as soon as possible would be everybody’s preference, Mendonça said, but that’s going to be challenging. Registered nurses working in hospitals and other medical settings can make $10,000 to $20,000 more than school nurses, and they are in even greater demand now because of the delta surge.
Hogan had hoped her state’s share would be used to hire another nurse at her high school. That would have allowed her and a partner to address COVID-19 as a team, while still conducting annual vision and hearing screenings, flu shot drives and other services for students.
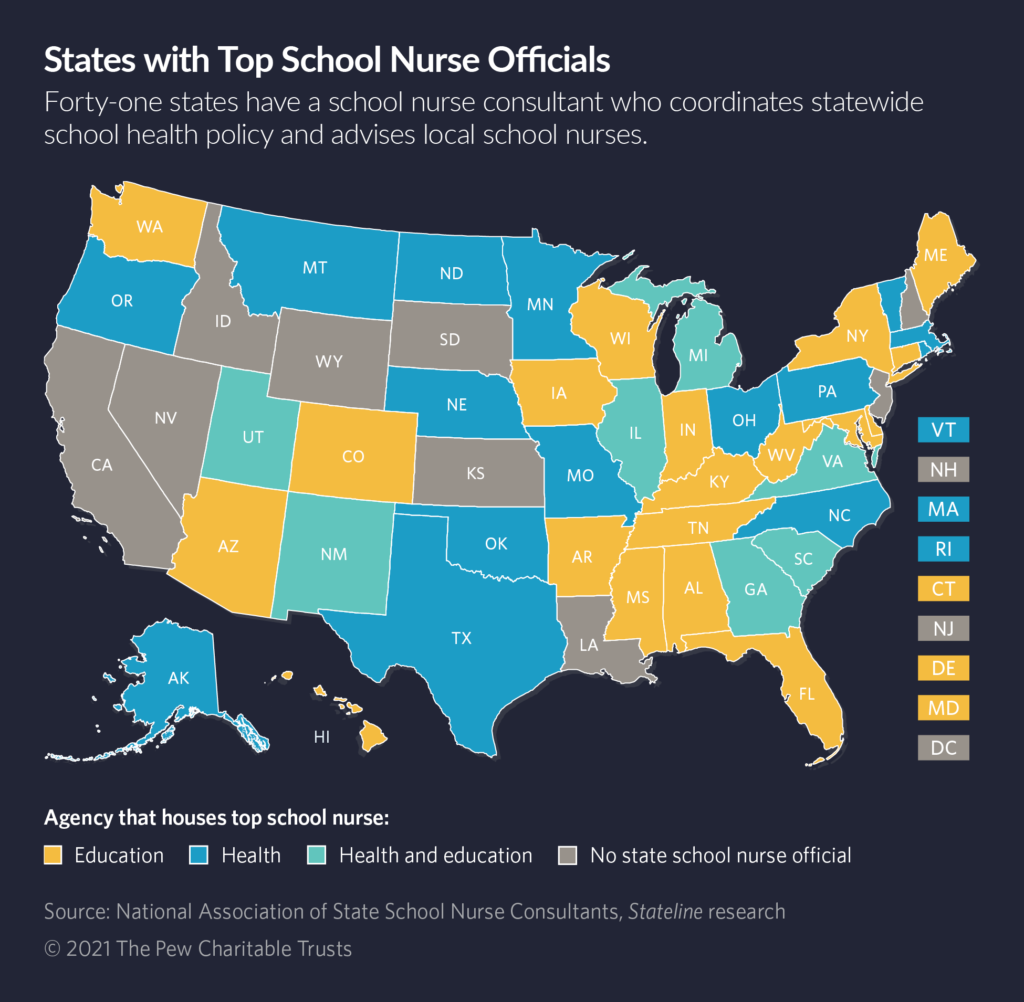
Instead, Maine’s public health agency plans to spend the new money on a telehealth contract and school-based health assistants with minimal health care training to fill in for school nurses while they’re busy juggling COVID-19 cases, said Emily Poland, Maine’s top school nurse official and president of the National Association of State School Nurse Consultants.
States applied to the federal Centers for Disease Control and Prevention for their share of the American Rescue Plan in September, and the money will flow to states this year and next.
In their applications, Poland said, some states said they plan to use the funding for school nurse scholarships and mentoring programs to develop a stronger workforce.
Other states are slated to use the money on support personnel for existing school nurses, such as state and regional experts to advise school nurses on managing chronic diseases, deciphering new CDC guidance and addressing emerging health issues that affect school-age children.
To free up more of existing school nurses’ time so they can work with students one-on-one and help schools develop better nutrition and exercise programs, some states plan to use the new federal money to reduce administrative chores such as billing Medicaid and Medicare for certain services.
“State health officials would be very enthusiastic about having more nurses in schools,” said Dr. Marcus Plescia, chief medical officer of the Association of State and Territorial Health Officials. “I understand there’s a nursing shortage, but some nurses may be attracted to school nursing programs. The pace is different, and they wouldn’t be dealing as much with sick patients.”
With a stronger bench of nurses in schools, Plescia said, they could get more involved in preventive care and wellness programs. They also could contribute more to public health by acting as eyes and ears on the health of the local population, since many illnesses first start to show up in schools, he said.
Diminishing Workforce
The roster of school nurses charged with protecting the health and well-being of the nation’s more than 50 million K-12 students and their teachers was already meager before the pandemic.
In the past year, retirements and resignations tied to burnout thinned their ranks even further, Mendonça said.
The American Academy of Pediatrics and the school nurses association recommend having at least one registered nurse in every school.
But with just under 96,000 registered nurses employed in public schools, fewer than 40% of the nation’s public schools have a full-time nurse, according a 2017 survey from the National Association of School Nurses. (A new survey will be taken this year.)
At least 25% of schools have no nurse and 35% have only a part-time nurse, the survey found.
At the same time, the registered nurses who could fill those positions were in short supply before the pandemic and the deficit has deepened since. More than 500,000 registered nurses are expected to retire by 2022, creating a need for 1.1 million more nurses, according to the American Nurses Association.
“Before COVID, school nurses’ responsibilities were vast,” Mendonça said. “They helped students manage chronic diseases such as asthma and diabetes and detected the early warning signs of kids in crisis.”
But since the pandemic began, the jobs of school nurses have been overtaken to fight the spread of the virus.
“They’re finding this year much more challenging than last year,” Mendonça said. “In 2020, everybody went home. This year, they’re back in school and everyone is stressed, tired and challenged with the ever-changing landscape of this pandemic. The delta variant changed everything.”
Before the American Rescue Plan money became available, some states and localities spent their own funds on contract nurses from local hospitals and other efforts to help school nurses get through the pandemic.
Maine, for example, hired a nurse for every county that school nurses could contact for guidance during the fast-paced changes in COVID-19 protocol last year.
Contact Tracing
At a news conference organized by the local teachers union this month, nurses in the Columbus, Ohio, school system said contact tracing COVID-19 cases was consuming so much of their time that they were unable to safely address all of the other health care needs of the students, according to a report in the Columbus Dispatch.
School nurses everywhere are voicing similar concerns and frustrations, said Kate King, school nurse at World Language Middle School in Columbus and president-elect of the National Association of School Nurses.
“COVID-19 cases are falling solely on school nurse, leaving them little time to do all of those other things they do,” she said in an interview with Stateline.
“Of course, we would never leave a student in a crisis,” King said. But screening, chronic disease management, behavioral and mental health care, longer-term wellness planning, and all of the other school nurses’ duties are getting short shrift, she said.
In Maine, Hogan’s high school of 725 students and 150 adult employees has reported only four positive COVID-19 cases since school opened in September. The Maine health department recorded 2,916 cases in all the state’s schools in its latest 30-day report published Oct. 21.
Still, it’s cold and flu season in Maine, and more kids are coming into Hogan’s office with headaches, sore throats, fevers, nausea, stomach aches and coughs. “They could all have COVID-19,” she said. “We don’t know until we test.”
“When any student shows up with symptoms that could be COVID, there’s a snowball effect of calling parents, giving them information about quarantining, calling for a COVID test, walking the student out to the car—it’s a time-consuming process.”
Janis Hogan, school nurse in Maine
After one student reported COVID-19-like symptoms and tested positive two weeks ago, Hogan said, she and two assistant principals worked for an entire day to track down the kids he was in close contact with.
They had to determine how many classes he was in and whether he rode the bus, played sports or ate in the lunchroom. Initially, they identified 200 close contacts and then used seating charts to determine who sat farther than 6 feet away. They ended up with 95 students in close contact with the student, eliminated those who had been vaccinated, and arrived at 28 students who had to be quarantined outside of school.
“When any student shows up with symptoms that could be COVID,” Hogan explained, “there’s a snowball effect of calling parents, giving them information about quarantining, calling for a COVID test, walking the student out to the car—it’s a time-consuming process.”
On top of that, Hogan said, “Parents often say, ‘It’s only a cold. Why can’t my kid come back to school?’”
This year, online classes aren’t an option for Camden Hills Regional High School students who must quarantine.
Even when a student in quarantine gets a negative COVID-19 test, Hogan said, “I have to tell the parents, ‘Thanks for the negative test, but please keep your kid at home until his symptoms are gone. Even a minor cold that gets spread around the school can result in weeks of contact tracing work.’”
Stateline, an initiative of The Pew Charitable Trusts.


