Phoebe Holdenson Kimura, University of Sydney and Bianca Cannon, University of Sydney
Around one in four women of reproductive age experience heavy periods, also known as heavy menstrual bleeding. Periods are a very personal experience and women (and people with uteruses) who have had heavy periods for a long time will often consider this normal, or something to be simply put up with.
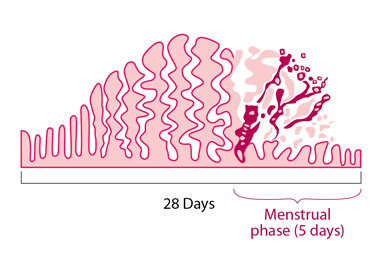
A woman with normal periods loses between six to eight teaspoons of blood with each period. On average, bleeding lasts for five days, but a normal period can last for up to eight days. Trying to work out the amount of blood loss can be tricky, but if you have any of these symptoms you probably have heavy periods:
- bleeding through clothing
- having to change pads and tampons every one to two hours
- passing clots larger than a 50 cent coin
- avoiding leaving the house on the heaviest days
- periods that interfere with your physical, emotional, or social life.
Many women with heavy periods also experience severe period pain. If you are having heavy periods, talking with your doctor can help you choose the right treatment option for you.
Causes
Heavy periods are most often caused by:
- hormone-related problems. Causes include perimenopause, polycystic ovarian syndrome, or thyroid conditions
- changes within the uterus (womb), such as fibroids or polyps (benign tissue growths from the wall of the uterus). Less commonly, cancer or precancerous changes may be the cause of heavy bleeding. Some of the red flags doctors look for are sudden changes in bleeding patterns or vaginal bleeding after menopause
- blood disorders.
Some women can have more than one contributing cause. However, around half of women with heavy bleeding will not have any recognisable cause, even after testing. Nevertheless, the symptoms will still need treating.
Tests
All women with heavy periods need to have some tests performed to establish the potential cause of their bleeding, and to guide the treatment options. This may include a:
- physical exam
- cervical screening test, if not up-to-date
- blood test to check for low iron levels, and possibly thyroid and clotting function
- pelvic ultrasound.
The doctor may suggest further tests, such as a test for chlamydia, pregnancy or a biopsy of the uterus.
Treatments
Don’t just put up with heavy periods, there are now many good treatment options.
You can consider starting initial treatment for heavy bleeding before your first visit to the GP. Oral non-steroidal anti-inflammatories such as ibuprofen or naproxen can be taken regularly from the first day of the period for up to five days. Many women are aware anti-inflammatories treat period pain, but they can also decrease the volume of bleeding by up to 50%.
Another oral treatment for heavy bleeding which may be prescribed by your GP is tranexamic acid. This is taken for the first four days of the period. Anti-inflammatories and tranexamic acid can also be taken together.
Another effective medical treatment is the hormone-releasing IUD (brand names Mirena and Kyleena). These provide reliable contraception and reduce bleeding. These can be inserted by a GP who has experience in IUD insertion, by a family planning clinic, or by a gynaecologist.
Oral hormonal options for treatment include the combined oral contraceptive pill or progesterone tablets.
Another important part of treating heavy bleeding is replacement of iron stores if you’re deficient. You can try to increase your dietary iron intake, but your GP may also recommend oral iron supplements. These can cause side effects such as constipation or nausea, so your GP may recommend an iron infusion instead.
Do I need to see a specialist?
Your GP may refer you to a specialist if there are red flags, an abnormality on the pelvic ultrasound or if the bleeding doesn’t improve after six months of trialling treatment.
The gynaecologist may offer a hysteroscopy, where a camera is inserted into the uterus. This can be used to treat abnormalities such as fibroids or polyps.
Endometrial ablation, where the lining of the uterus is purposefully damaged, can be used to reduce or completely cease monthly bleeding. But it’s not suitable for women who are planning a future pregnancy.
The final option for treating heavy bleeding is surgical removal of the uterus via hysterectomy. Historically, this was often used due to a lack of other treatments. While it does permanently resolve heavy bleeding, it has more risks than the other treatments, and is obviously not suitable for women who still wish to bear children. Hysterectomy is considered when other treatments are ineffective or inappropriate, or at the patient’s request.
5 tips for getting help for heavy periods
- Don’t delay. See your GP if you think your periods are heavy or if they’re interfering with your work or personal life
- keep a diary of symptoms and track your cycle to help your GP understand your periods. Jot down some notes, fill out a period tracking chart or use a free app to keep track
- allow enough time. Make an appointment specifically to discuss your heavy periods and get answers to any questions you have. Consider making a double appointment
- don’t be embarrassed to discuss your symptoms or ask your GP questions. This is a common and important problem
- go back for review if your bleeding isn’t improving after starting treatment. It might be time to discuss other options.
Phoebe Holdenson Kimura, Lecturer and GP, University of Sydney and Bianca Cannon, GP and Lecturer at Sydney Medical School, University of Sydney
This article is republished from The Conversation under a Creative Commons license.
Read the original article.


