By Luisel Ricks-Santi, University of Florida
“Me encontraron càncer en la pròstata,” my father told me. They found cancer in my prostate.
As a cancer researcher who knows very well about the high incidence and decreased survival rates of prostate cancer in the Caribbean, I anguished over these words. Even though I study cancer in my day job, I struggled to take in this news. At the time, all I could muster in response was “What did the doctor say?”
“The urologist wants me to see the radiation oncologist to discuss ‘semillas’ [seeds],” he said. “They are recommending treatment.”
However, I understood from my work that not undergoing treatment was also an option. In some cases, that is the better choice. So I took it upon myself to educate my father on his disease and assist him with the life-changing decisions he would have to make. Our journey can give you a preview of what a cancer diagnosis can be like.
Prostate cancer diagnosis
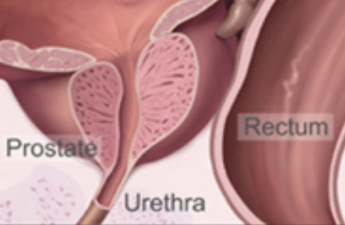
Prostate cancer was not a new topic for my father and me. His battle with his prostate health started 10 years ago with an initial diagnosis of benign prostate hyperplasia, or BPH.
The prostate gets bigger with age for a number of reasons, including changing hormone levels, infection or inflammation. Two of the most frequent symptoms of BPH are difficulty urinating and a sudden, urgent need to urinate, both of which my father experienced.
Although research suggests that the factors that contribute to BPH similarly contribute to prostate cancer, there is no evidence that an enlarged prostate will necessarily develop into cancer. https://www.youtube.com/embed/_Jcq4FDTheg?wmode=transparent&start=0 Prostate cancer diagnoses have risen in the U.S. in recent years.
Upon my father’s initial BPH diagnosis, I asked about his PSA levels, or the amount of prostate-specific antigens in his blood. PSA is a protein that both normal and cancerous prostate cells produce, and elevated amounts are considered red flags for prostate cancer. When combined with a digital rectal exam, a PSA test can allow doctors to more accurately predict a person’s risk of having prostate cancer.
My father said his PSA levels were elevated but that the doctors would begin active surveillance, or what he called “watchful waiting,” and monitor his PSA every six months to see if it rose.
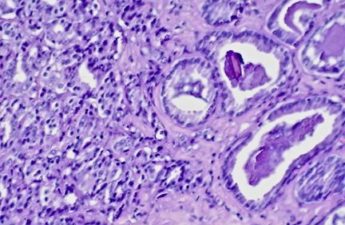
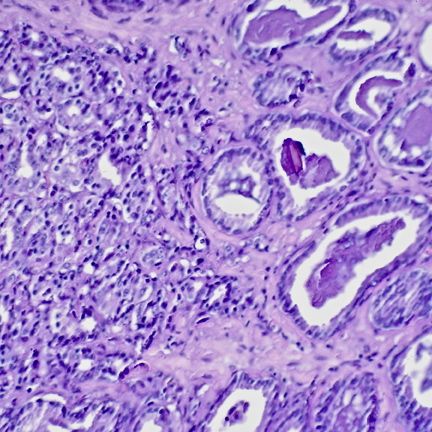
After eight years of monitoring his PSA, doctors found my father’s PSA level had doubled. He then got a biopsy that indicated he had intermediate-risk prostate cancer.
Cancer risk categorization
After his diagnosis, my father was faced with the decision of how to proceed with treatment. I explained that categorizing how aggressive the cancer is and how far it has spread can help determine the best course of treatment.
Prostate cancer can be grouped into four stages. Stages 1 and 2, when the tumor is still confined to the prostate, are considered early-stage or intermediate risk. Stages 3 and 4, when the tumor has spread beyond the borders of the prostate, are considered more advanced and high risk.
Some patients with early-stage or intermediate-risk prostate cancer undergo additional treatment, including surgery, radiation or radioactive seed implants called brachytherapy. Patients with late-stage prostate cancer typically undergo hormone therapy along with surgery or radiation, or chemotherapy with or without radiation.
Although I was not surprised by my father’s diagnosis, given his advanced age and his battle with prostate disease over the past decade, I still struggled emotionally. I struggled with our conversations about what “curing” his cancer meant and how to explain his treatment options to him. I wanted to ensure he would have the best outcome and could still live his best life.
Our initial inclination was to undergo active surveillance. That meant we would monitor his PSA every six months instead of immediately starting treatment. That is appropriate for patients with early-stage and less aggressive tumors.
Prostate cancer screening problems
My father was leaning on me to help him decide how to proceed. I felt overwhelming anxiety because I did not want to fail him or my family. Even with all my expertise studying cancer genetics and working with cancer patients, I couldn’t help second-guessing our decisions, and I sometimes questioned our decision not to immediately treat his cancer.
Some people diagnosed with prostate cancer don’t immediately start treatment, because many of the tumors found through PSA testing grow so slowly that they are unlikely to be life-threatening. Detecting these slow-growing tumors is considered overdiagnosis, because the cancer ultimately will not harm the patient during their lifetime. Nearly half of all patients with prostate cancer are overdiagnosed, often leading to overtreatment.
Research suggests that many prostate cancer patients undergo unnecessarily aggressive treatments, which are often associated with significant harms, like urinary and bowel incontinence, sexual impotence and, in some cases, death. Several studies in the U.S. have shown that patients with early-stage prostate cancer have a good prognosis, and the cancer rarely progresses further. With careful observation, most will never need treatment and can be spared the burdens of unnecessary therapy until there are clear signs of progression. https://www.youtube.com/embed/tYii98gcejA?wmode=transparent&start=0 The U.S. Preventive Services Task Force recommended individualized PSA-based screening in 2018 to avoid overdiagnosis and overtreatment.
Overdiagnosis and overtreatment of prostate cancer led the U.S. Preventive Services Task Force to recommend against PSA-based screening in 2012, with caveats for high-risk groups including African American men and those with a family history of prostate cancer. The recommendation was updated in 2018 to make screening a personal choice after discussion with a clinician.
Those recommendations have resulted in reduced screening and increased prostate cancer diagnoses. Given that Black men are more likely to see the cancer progress to aggressive forms of the disease after initial diagnosis, this may worsen existing health disparities.
Developing tests that better identify patients at risk of dying from prostate cancer can decrease overtreatment. In the meantime, educating patients can help them decide if screening is appropriate for them. For underserved and marginalized communities, community outreach can help improve health literacy and enhance awareness and screening.
When I looked through my father’s stack of medical records, I found a beacon of light that eased my apprehension. His doctor had ordered a genetic test that estimates how aggressive a tumor may be by measuring the activity of specific genes in cancer cells. An increase in gene activity linked to cancer would indicate that it is likely to grow fast and spread.
The test predicted that my father’s risk of dying from the disease in the next five years was less than 5%. Based on these results, we both understood that he had adequate time to make a decision and seek additional guidance.
My father ultimately decided to continue active surveillance and forgo immediate treatment.
Surviving prostate cancer
I still worry about my father’s diagnosis, because his cancer is at risk for progression. So every six months, I inquire about his PSA levels. His doctors are monitoring his PSA levels as part of his survivorship plan, which is a record of information about his cancer diagnosis, treatment history and potential follow-up tests.
My father’s decision to undergo active surveillance was controversial among our friends and family. Many were under the impression that prostate cancer required immediate treatment. Several shared successful treatment stories, sometimes followed by stories of adverse treatment-related side effects.
To date, my father believes that active surveillance was the best decision for him and understands that this may not be the same for someone else. Talk to your doctor to see what the best options are for you or your loved ones.
Luisel Ricks-Santi, Associate Professor of Pharmacy, University of Florida
This article is republished from The Conversation under a Creative Commons license.
Read the original article.