January 1, 2025 by Claudia López Lloreda
When the Covid-19 pandemic first struck, Christopher Chiu and other researchers wondered: Should they inject healthy people with the virus that caused the pandemic?
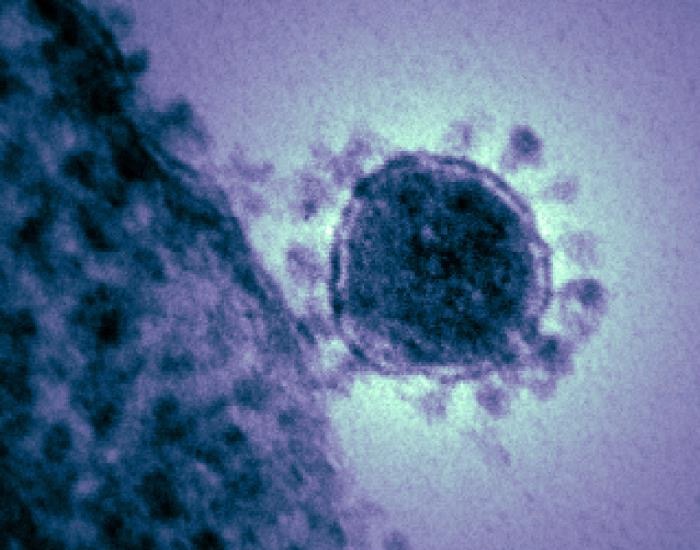
The idea sounded counterintuitive, but by carefully dosing individuals with SARS-CoV-2 in a controlled setting — like Chiu had been doing for more than a decade with seasonal flu and RSV — scientists could study how the virus affects the body and learn what factors may offer protective benefits.
These types of studies, called human challenge trials, could help fast-track understanding the deadly virus devastating the world, experts claimed. Others, though, questioned whether the potential benefits were worth the risk, particularly given the host of unknowns surrounding Covid-19, and the lack of available treatments at the time.
After months of deliberation among doctors, scientists, ethicists, and regulators, the world’s first Covid-19 human challenge study was ultimately born in early 2021. And Chiu, an infectious disease physician and immunologist at Imperial College London, was its chief investigator: “We sort of recognized that there were still lots of things we didn’t know about how the disease happens.”
Early insights helped guide U.K. public policy on isolation times. Nearly four years later, more results are starting to emerge: One recent study published in eClinicalMedicine, one of the Lancet’s open-access journals, suggests individuals who got infected performed worse on cognitive tests than those who didn’t — a finding that may speak to long Covid and the cognitive effects of infection but which has received pushback from other experts. Another 2024 study points to a protein that might help protect against Covid-19. And the most recent study found that certain blood biomarkers may help researchers stratify patients for different treatments.
“There were still lots of things we didn’t know about how the disease happens.”
Christopher Chiu, Imperial College London
For Chiu, these studies were a success. And researchers continue to conduct challenge trials with the goal of developing better vaccines than the ones on the market and now want to expand trials to other countries.
Yet some skeptics argue none of these challenge trials were necessary, and that many of the findings could have been gleaned through other types of studies. The challenge trials, for instance, didn’t directly inform vaccine or treatment development, raising questions about whether these risks were justified.
“Did we really learn?” said Marc Veldhoen, an immunologist at the University of Lisbon and Gulbenkian Institute for Molecular Medicine. “Not so much.”
Human challenge trials have been going on in some form since the 1700s — and they’ve long been controversial. In recent decades, the trials have become more scientifically rigorous but have continued to spark ethical concerns surrounding potential risk and subject exploitation.
Still, they have persisted due to several key advantages.
For one, because researchers control the type of virus and dose, they’re able to better attribute cause to effects. “If a patient does something weird or has a unique response, you never know why that exactly is. Is it because of comorbidities? Is it because this person happened to have been exposed to a massive dose?” said Rik Lindeboom, an immunologist at the Netherlands Cancer Institute in Amsterdam. “With these challenge studies, you can really control for all of this and that makes them very, very unique.”
In recent decades, challenge trials have become more scientifically rigorous but have continued to spark ethical concerns surrounding potential risk and subject exploitation.
Scientists can also control the time of exposure, allowing them to pinpoint how long it takes for someone to become infectious and develop symptoms. Indeed, one of the first Covid-19 challenge trial papers, published in 2022, found that individuals started to shed SARS-CoV-2 after just two days of infection and that they could remain contagious for another 10. Participants with a negative Covid-19 test were not shedding virus, they also found.
At the time, this information had a direct impact on public health decision-making in the U.K., said Chiu, and led to the recommended isolation period of 10 days: “With this research, we were able to really clearly define when you could come out of self-isolation.” Other studies revealed that some people naturally shed large amounts of virus and that people’s bodies fight off infection by increasing an immune pathway called the interferon response, providing a potential target mechanism to help reduce transmission and disease.
More recently, challenge trials have given insight into a unique population that might otherwise not be studied: those who don’t get infected after exposure. In a Nature study published in June, Chiu and colleagues exposed 16 participants to SARS-CoV-2, yet only six developed a sustained infection. Then, Lindeboom studied the immune cells from these participants and found that the people who avoided infection all shared a high expression of a gene the researchers think could potentially protect against infection, said Lindeboom.
Meanwhile, the recent eClinicalMedicine study compared infected and uninfected participants on a set of cognitive tests. The 18 infected participants performed worse than the 16 who did not become infected, particularly in tests that measured memory and executive function. These changes persisted for at least a year, suggesting that the virus could have lasting effects on cognitive function.
That study, though, has received some criticism. Veldhoen, the immunologist in Lisbon, pointed out that the differences between the groups were variable and modest. “If you look at all the tests individually, I think there’s only one or two where there is indeed a difference — the difference is quite small,” said Veldhoen, noting that when it comes down to whether the work was necessary, he is “still not completely convinced.”
Indeed, not everyone agreed that the challenge trials were worth the risk. For example, U.S. institutions decided not to approve such trials, in part because, at the time, clinicians lacked an effective treatment for severe cases — typically a key consideration in conducting challenge trials. And while none of the studies conducted to-date have reported serious adverse events such as hospitalizations, some experts question whether more challenge trials are worth the gamble, particularly given the question marks surrounding long Covid.
The decision to infect someone with a pathogen needs to be outweighed by clear and obvious benefits, said Angela Huttner, an infectious disease physician at Geneva University Hospital. “If you’re going to sacrifice one person, it better be for the good of more than one person,” she said. Before the studies were conducted, she and others thought that Covid-19 failed to meet those criteria. Now the lack of what they consider meaningful results confirms their worries.
Meanwhile, some experts say that challenge trials may not be necessary given the prevalence of Covid-19. In the United States, “we were able to conduct the huge Phase 3 trials with 30-40,000 participants per vaccine,” wrote Kirsten Lyke, an infectious disease specialist at the University of Maryland, in an email to Undark.
“If you’re going to sacrifice one person, it better be for the good of more than one person.”
By comparison, challenge trial studies typically attract fewer than 100 subjects. The 2022 Nature study, for example, included just 36 young and healthy volunteers. Veldhoen noted that the small sample size limits the research’s statistical power and generalizability: “It’s super difficult to get the bigger picture from those studies,” he said. Huttner agrees: “You can glean some information, but it may be clinically very limited.”
The findings also did not result in a new vaccine or treatment, as some experts have pointed out. “I’m not convinced that Covid-19 human challenge models turned out to be critical to the effort to develop biologics, vaccines and therapeutics,” Lyke wrote in her email.
Chiu, meanwhile, argues that although current vaccines effectively prevent serious disease and death, they are subpar in stopping the spread. Challenge trials, he said, can help develop better vaccines.
In fact, Chiu leads a new initiative that intends to do just that: The Mucosal Immunity in Human Coronavirus Challenge, or MusiCC, project has received $57 million to develop experimental vaccines to block transmission. The global consortium also aims to increase the capacity to conduct challenge trials worldwide, Chiu said.
Chiu and a group of collaborators at the University of Oxford led by Helen McShane, an infectious disease physician, are also now recruiting for their next challenge trial in which they will infect participants with the Omicron strain. Meanwhile, another research group in Singapore is currently recruiting for a study on the Delta variant.
While some experts have dismissed insights gleaned from the last few years of challenge trials — “We haven’t learned something that we wouldn’t have gotten in another way,” said Veldhoen — justification for the trials looks different for Chiu.
“It is subjective how much you think scientific findings are worth and their value and their potential impact for the future. So, again, it’s always a conversation to be had, and I would never sort of stop people from criticizing,” he said. “Each new study is a new discussion, and you have to weigh things up again.”
This article was originally published on Undark. Read the original article.



