This decrease could lead to fewer doctors in less populated areas of the country

By by Lauren Baggett, University of Georgia
Rural America is running short on physicians. This worries health experts who have linked limited access to primary care providers to major gaps in health outcomes for rural communities.
Addressing this issue is complicated, but new research from the University of Georgia suggests that understanding geographic trends in medical school applicants could help project where the future physician workforce is likely to practice.
Knowing a medical student’s hometown is an important piece of the puzzle, said study author Donglan “Stacy” Zhang, because geography is known to predict where many new doctors choose to practice.
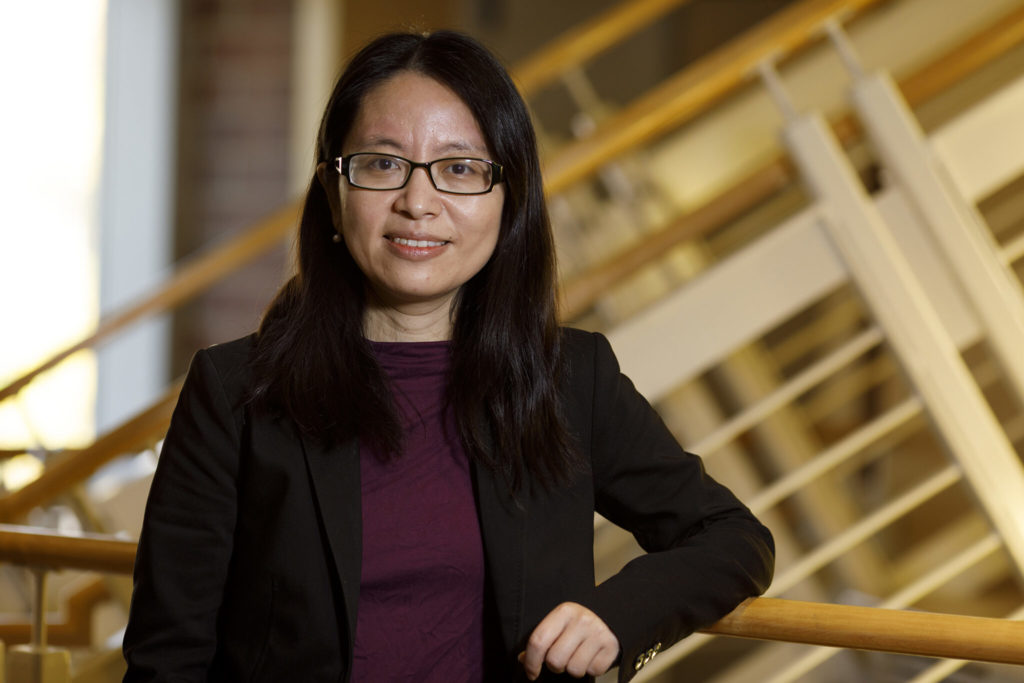
“More than 60% of doctors choose their practice location in their birth state, as well as where they attend medical schools or residency program training,” said Zhang, an assistant professor of health policy and management in UGA’s College of Public Health.
“Having a lower number of medical applicants from a lower-resourced region could mean fewer future doctors providing health care in these areas,” she said.
Rural medical applications dropped
To find out if this prediction was accurate, she and colleagues in the College of Public Health and the Department of Geography in UGA’s Franklin College of Arts and Sciences analyzed trends in medical school applications and matriculation between 2001 and 2015, tracking not only where applicants came from and how that changed over time, but what factors drove those changes. In addition, the team looked at the applicants’ proximity to a medical school.
They found that applications have climbed steadily over time, but the number of applications coming from rural or remote areas has dropped.
“We also found that the number of counties without any applicants was increasing during the past 15 years, with the majority of these counties, between 60% and 70% being low-income or middle-low-income,” said first co-author Gang Li, a doctoral student in the College of Public Health.
Reasons for the decrease
Zhang attributes this to multiple factors, all tied to socioeconomic status.
“Students from lower-resourced families and regions have fewer educational opportunities to begin with. For example, they have limited access to quality public schools or local colleges that likely hinder their pursuing higher education. Even when they show the potential to be successful in medical education, financial constraints significantly affect their decisions to attend medical school,” said Zhang.
The researchers also found that applicants tended to live near a medical school, which makes sense given the consolidation of health care facilities, medical schools and higher income families to urban settings.
Potential solutions to doctor shortages
There are some states and medical schools that have offered tuition waivers or invested in residency programs in underserved communities to attract physicians to practice in those communities, and this is a start, but Zhang emphasizes that addressing the underlying socioeconomic disparities is critical to ensuring future primary care options for rural areas.
“Some complementary and bold policies are necessary,” said Zhang.
Investment in needs-based free tuition is one option, she said. In addition, primary care roles could be filled by international medical graduates, doctor of osteopathic medicine program graduates, nurse practitioners, and physician assistants – all programs that could be more accessible to a broader set of applicants.
The study, “Trends in Medical School Application and Matriculation Rates Across the United States from 2001 to 2015: Implications for Health Disparities,” was published recently in Academic Medicine. The paper is available online here.