Public Health investigates HIV infection in heterosexuals who inject drugs
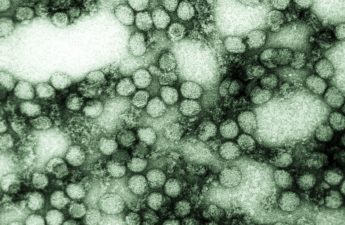
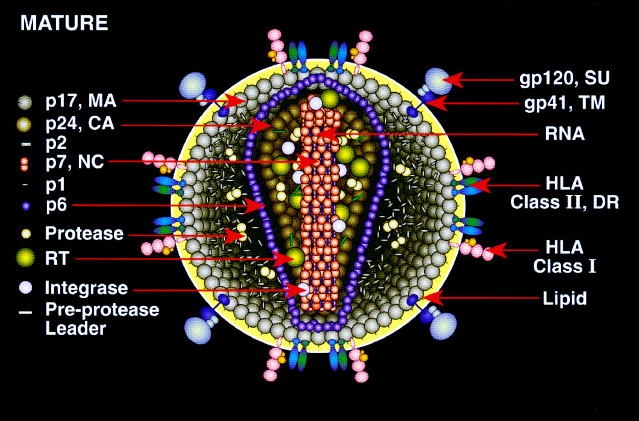
Public Health – Seattle & King County has recently identified an increase in the number of new HIV cases among heterosexuals who inject drugs in King County. HIV infection is typically much less common among heterosexuals in King County than among men who have sex with men (MSM). But the risk for HIV infection increases among people who use injection drugs.
Specifics on new HIV cases
Since February of this year, Public Health has identified a cluster of eight people with HIV infection in north Seattle. Public Health discovered these cases through a combination of routine HIV testing, investigation of newly reported cases and HIV testing outreach efforts. All people in the cluster were living homeless and injected or used illicit drugs; several reported exchanging sex for money or drugs.
Driven by this cluster, local public health officials are concerned that new cases among heterosexuals who inject drugs, as well those having unprotected sex with people using injection drugs or exchanging sex for money or drugs, could increase if steps are not taken to limit the spread of infection.
To date, 19 heterosexuals who inject drugs have been diagnosed with HIV in King County in 2018. Over the past 10 years, an average of 10 heterosexual people who inject drugs were diagnosed with HIV in the county annually, with seven diagnosed in 2017.
Locally, among people who inject drugs, methamphetamine use has been more closely linked to HIV infection than opiate use. However, individuals injecting drugs in King County increasingly use both drugs, and all of the recently identified cases occurred in people who have used both opioids and methamphetamine. Overall in King County, approximately 2% of heterosexuals who inject drugs are HIV infected.
“This cluster is unusual and worrying, suggesting that we are seeing an increase in HIV among heterosexuals who inject drugs, and that HIV could be gaining inroads into the heterosexual population through injection drug use,” said Dr. Matthew Golden, MD, Director of Public Health’s HIV/STD Program. “Changes in drug use patterns, with greater mixing between heroin users and people who inject methamphetamine, may be putting more people at risk for HIV.”
Homelessness is a contributing factor for HIV as well as other communicable diseases; people experiencing homelessness have a high prevalence of injection drug use, behavioral health challenges and poor access to health care. Unprotected sex is also a high risk factor for HIV transmission, especially with multiple partners and including partners using injection drugs.
Protecting the community
“The most effective way to prevent HIV transmission in the community is to identify people with HIV, link them to medical care and ensure that they are treated,” said Dr. Jeff Duchin, Health Officer for Public Health – Seattle & King County. “Medications for HIV suppress the infection, safeguarding the health of infected persons and preventing HIV transmission.”
King County was among the first counties in the nation to achieve the World Health’s Organization 90-90-90 objective (i.e. 90% of infected persons diagnosed, 90% of diagnosed persons in care, and 90% of those in care virally suppressed). Local public health officials estimate that over 90% of those who are in care are virally suppressed and therefore cannot transmit HIV.
To address the current cluster of cases and decrease the risk of more HIV transmission, Public Health is:
- increasing outreach and testing programs, working closely with local health and social service providers to ensure that prevention messages reach those at risk and that testing is readily available to persons who may be at-risk for infection.
- providing case management for individuals newly-identified with HIV and linking them to treatment services.
- alerting healthcare providers and urging them to increase HIV testing and prevention counseling for those at-risk. Several local hospitals are also increasing testing in emergency departments.
- continuing to assure access to sterile injection equipment and condoms through needle exchanges, and provided direct education to impacted communities.
Guidance for local providers
Medical and social service providers who serve people who inject drugs, who are living homeless or who exchange sex for drugs or money should counsel their patients and clients to get tested for HIV and syphilis frequently, to avoid sharing injection equipment and to use condoms regularly.
Healthcare providers should also discuss pre-exposure prophylaxis (PrEP) with people who inject drugs in order to prevent HIV infection.
Continuing response
The ability to detect and respond to an increase in HIV infections among heterosexuals highlights the importance of a robust public health system and close working relationships with community partners.
At this time, local public health officials do not know if the recently identified cluster will be an ongoing and significant change in local HIV transmission patterns compared to past years. Public Health will continue to monitor the situation, and take additional steps as needed to decrease the risk of further HIV spread in our community.
Look to the Public Health Insider blog for an update next week as the response continues.
Originally posted on August 30, 2018.