World AIDS Day: An update on HIV in King County
Each year, World AIDS Day is a chance to take note of our successes, on-going challenges and opportunities responding to the HIV epidemic. World AIDS Day this year is December 1st. While the news is good in important areas, there are troubling issues as well. We sat down with Dr. Matthew Golden, MD, HIV/STD Control Officer for Public Health – Seattle & King County to learn more.
Dr. Golden, it’s been a busy year in the HIV/STD program. What are some of your key successes?
Our biggest news is the ongoing reduction in new HIV diagnoses in King County. Last year 161 King County residents were diagnosed with HIV, the lowest number since 1994. This is a 51% decrease in new HIV diagnoses overall and a 58% decline among men who have sex with men (MSM) over the past 10 years.
We attribute this decline in HIV to the success of HIV treatment, as well prevention interventions such as PrEP (drugs that prevent HIV) and needle exchange. To our knowledge, King County was the first urban area in the U.S. to achieve the World Health Organization’s goal of ensuring that at least 90% of infected persons know their HIV status, that 90% of infected people are treated and that at least 90% of treated persons are virally suppressed.
What has contributed to these results?
A lot of things contributed to our success. People with HIV benefited from the Affordable Care Act, Medicaid expansion, and sustained federal funding through the Ryan White Program, all of which have been essential in ensuring that they can access health care, including medications to keep HIV infections under control. We also have a superb medical system – with great clinicians throughout our community and in places like Harborview’s Madison Clinic and Max Clinic and Public Health’s STD clinic – and outstanding prevention providers at community-based organizations.
Question: Decreases in MSM case rates is really great news. But last summer you told the Insider about cases among non-MSM who inject drugs. Where does that stand?
Over the last year, we have seen a big increase in the number of HIV cases diagnosed among non-MSM (e.g. heterosexuals, bisexuals, or lesbians) who inject drugs. We usually have 7-10 new diagnoses per year in King County among non-MSM who inject drugs. So far this year we’ve had 27, which is about a 300% increase. This is a major concern and something we have never really confronted before in King County.
How does that relate to the cases we talked about last summer?
We first noted the increase in HIV among persons who inject drugs when we identified a cluster of cases among persons who were living homeless in north Seattle, most of whom used injection drugs and many of whom exchanged sex for money or drugs. As of November 26th, the cluster includes 14 people with HIV diagnosed in 2018, 12 of whom inject drugs.
Using genetic fingerprinting, we traced the history of the strain of HIV impacting the people in the cluster back over the past decade and found eight people who were diagnosed with a related strain of HIV between 2008 and 2017. So it seems like there was a low level of transmission going back about a decade, but that transmission in that group really took off in the last year.
So what’s the bottom line?
The bottom line is that while the cluster is among people with features in common – a sort of hot spot – the underlying problem is bigger than that and may be county-wide. Non-MSM who inject drugs and their sex and syringe-sharing partners are being infected at much higher numbers than we’ve seen in recent years in King County.
The good news is that the majority of people who inject drugs whom we’ve identified have HIV are now receiving medical care and many of them virally suppressed, decreasing their risk of becoming ill with HIV as well as their risk of transmitting HIV to others. Our team at Public Health, as well as our partners around the country are working very hard to make sure that everyone we diagnose with HIV gets the medical care they need as quickly as possible.
Why are we seeing this increase in non-MSM infections?
We’re trying to understand the answer to that question. The opioid epidemic and more use of stimulants like methamphetamine may play a role, which we discussed in an Insider blog last year. The intertwined problems of the ongoing opioid epidemic, rising methamphetamine use and growth in numbers of persons living homeless further increase risk for transmission of HIV as well as other infections.
HIV outbreaks among injection drug users have also occurred elsewhere in the country, such as in Massachusetts and Indiana. Indiana had a big outbreak in 2014that occurred in a rural area with very limited prevention services and no needle exchange.
What are needle exchange programs like in King County?
We are fortunate that we have excellent syringe exchange services, and that has certainly helped keep our HIV infection rates low among people who inject drugs. At the same time, the current situation makes it clear that our longstanding prevention efforts were insufficient to prevent the current outbreak and we need to expand our activities. We are working hard to increase needle exchange and other prevention and treatment services in the cluster area as well as among persons who inject drugs throughout the county.
What can people do to reduce their risk of HIV and AIDS?
There are a lot of things people can do to protect themselves. The best way for injection drug users to protect themselves from HIV is to never share drug equipment—not just syringes, but also cookers, and cottons—and use condoms consistently. Persons who inject should also avoid backloading. (Backloading is sharing the contents of one syringe with another syringe.)
Of course, condoms are important for all sexually active people who are at risk of HIV. We also suggest that persons who inject drugs and other persons at elevated risk for HIV get tested for HIV at least once a year. And, persons at higher risk for HIV, including persons who exchange sex and who inject drugs or are living homeless, should be on PrEP. Information about medical providers who prescribe PrEP or assistance in paying for PrEP can find this information on our website.
Finally, there is increasing availability of medication-assisted treatment for opioid use disorder in King County. For information on treatment options near you, call the Washington Recovery Helpline at 866-789-1511, visit their and visit Stopoverdose.org.
Can you explain PReP – the new drugs that prevent HIV infection in the first place?
If you’re at risk for HIV you can get on a drug regime called PReP – it prevents HIV from taking hold in your body. PrEP is remarkably effective when taken regularly. There are programs to pay for PReP if you can’t afford it.
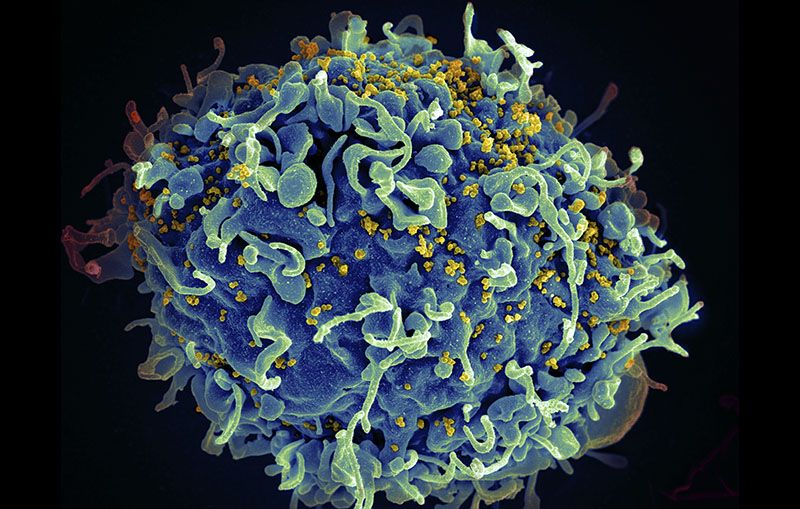
What is the outlook for people who do become HIV infected?
People with HIV live long lives now thanks to effective drug treatments. Every person in Washington state can get medication to treat HIV, regardless of ability to pay. Everyone. When people take HIV medications as soon as possible after infection and take their medications regularly, their risk of developing AIDS goes dramatically down. The newest drugs are easy to take—often only one pill per day—and have few adverse side effects. In fact, most people have no side effects.
What is next for your staff as you try to limit the spread of HIV in this non-MSM population?
We’re increasing outreach testing, needle exchange, condom distribution, linking infected people to medical care – including HIV treatment, PrEP and medication assisted therapy for substance use- and working with medical and social service partners to increase access to prevention and testing. We’re also helping make treatment for opioid use disorder widely available in King County.
Originally published on 11/30/18