Mylynda Massart, University of Pittsburgh
When I got home after work I was surprised to find my husband and three children sitting by the television and watching the news. They had just learned that the direct to consumer genetic testing company 23andMe was now offering a report that assessed the customers’ risk of developing Type 2 diabetes. “Is it true?” my husband asked. “Can they now study my genes and predict whether I will get Type 2 diabetes?”
As a primary care physician who is exploring how to integrate genetic testing into traditional family medicine – a combination we now describe as precision medicine – I was excited to explain the science behind this new report and the barriers to using 23andMe’s new diabetes risk score in current clinical care.
As a family physician, I am eager to identify my patients most at risk for developing diabetes, as this is a very costly and debilitating disease with numerous health consequences such as kidney failure, heart disease, painful neuropathy and limb amputation.
In the U.S. alone more than 30 million Americans have Type 2 diabetes and of these 7.2 million are undiagnosed and unaware of their condition. Another 84.1 million adults older than 18 are at high risk and considered prediabetic. So how did 23andMe calculate this risk score, and would it help the millions who were unaware of their state of health?
Calculating risk of Type 2 diabetes
As my family sat down to a carbohydrate-rich dinner of pasta, my famous pesto pizza rolls and a salad, I explained how this direct-to-consumer testing service was calculating the risk of this complex disease that is caused by the interaction of diet, environment and thousands of genes.
The piece of the puzzle that 23andMe is calculating is called the “polygenic risk score,” which is the likelihood we were born with of developing certain diseases or conditions.
Polygenic risk scores are not based on single genes or mutations. Instead, these calculations look at the cumulative effect of thousands of small variations scattered throughout our genomes. Not all variations cause harmful effects, some are beneficial and boost health, decreasing the odds of developing diabetes.
Each one of these variations alone may not have a significant impact on our health, but together they add up to increased risk of developing certain types of disease. According to 23andMe, the polygenic risk score for Type 2 diabetes was based on research using the shared DNA of their consumers.
The DNA data the company is collecting is not just to report results back to the consumer; some 2.5 million 23andMe customers have consented to allow the company to use their DNA for research. So can this polygenic risk score tell us our increased likelihood or susceptibility to developing diseases such as diabetes?
The short answer is yes.
With advances in genomics and large repositories of genetic data from the general public, scientists have now identified how certain genetic variants raise or lower risk of a particular disease and use these associations to calculate a risk score.
In an article published in Nature Genetics last year in 2018, the researchers reported polygenic risk scores that identified individuals with as much as three times the risk of developing Type 2 diabetes. That number certainly caught my family’s attention. This means that if your average risk as an American of developing a specific disease is 1 out of 100, then your new risk could increase to 3 out of 100.
That number certainly caught my family’s attention. This means that if your average risk as an American of developing a specific disease is 1 out of 100, then your new risk could increase to 3 out of 100.
Polygenic risk: Just part of the equation
While your genetics might actually tell you that you are at a higher risk for developing diabetes, that is not the whole story. In addition to genetic predisposition, it is important to factor in an individual’s environment.
When it comes to diabetes, the environmental factors are largely nutrition and activity. A diet low in sugar and carbohydrates, which I normally advocate for, when I am not feeding my family pasta, and an active lifestyle can override our genetic predisposition for diabetes. It can also control diabetes if it is diagnosed.
The key question, as researchers and physicians wrangle with incorporating more genetic data into health care, is how will individuals react to learning that they are genetically predisposed to developing diabetes? Will they use this knowledge to implement and sustain the lifestyle changes necessary to mitigate that risk?
Lifestyle changes like this are not easy. Many people make New Year’s pledges to exercise more and lose weight, but just two months into the year, some 80 percent of people fail to make those resolutions stick. We don’t know yet whether genetic knowledge will inspire people to commit to new lifestyles.
Won’t an annual check up detect developing diabetes?
You might be wondering: Can’t my primary care physician order lab tests to gauge my overall health and detect developing diabetes?
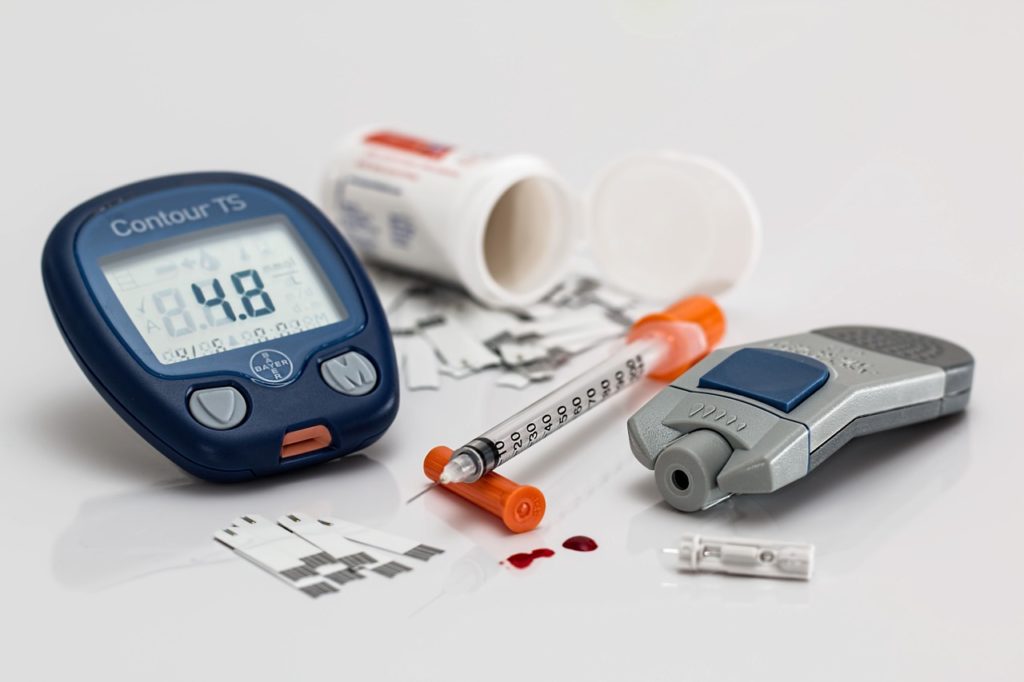
This is a great point. There are tests to measure for Type 2 diabetes. Conventional screening tests may include the monitoring of fasting blood sugar; measuring hemoglobin A1c and, occasionally, measurement of fasting insulin levels.
Unfortunately, by the time these biomarkers start showing changes consistent with pre-diabetes or the onset of diabetes, the disease process has already begun.
The screening tests allow us to react to the development of the disease, but a genetic test might help prevent the disease onset entirely. The promise of polygenic risk scores and their implications for health is exciting because it shifts the focus from diagnosis to prevention.
But that doesn’t mean that I will be recommending the 23andMe diabetes score instead of the regular laboratory A1c test. While the polygenic risk score test is exciting and sexy, it is not yet ready for prime-time clinical care. That’s because many health care providers don’t know what to do with this type of technology.
Barriers to genetic risk scores
There are still challenges to integrating genetics into primary care. The Food and Drug Administration, the government agency charged with overseeing these tests, has established that clinical decisions cannot rely solely on a direct-to-consumer genetic testing result, like the diabetes report, and that the result must be clinically validated in a clinical lab that processes routine testing.
Currently, there is not a FDA-approved clinical polygenic risk score test for diabetes that is universally available to health care providers. In addition, there is no defined space to store such genetic data in the electronic health record. The U.S. health care system also lacks evidence-based algorithms to guide providers how to use the data in clinical care.
So, what you do with your polygenic risk score? I recommend that when this test result does arrive, you share it with your PCP. Even though your doctor cannot use the test nor order its clinical counterpart at this time, you can both engage in ongoing discussions about how to improve your health with regular exercise and better food choices and continue with your scheduled preventative health care.
Remember, the next time your doctor says eat well and exercise, that might not be just good advice but actually a precision medicine prescription for your health.
Mylynda Massart, Assistant Professor of Family Medicine, University of Pittsburgh
This article is republished from The Conversation under a Creative Commons license. Read the original article.


