Helen Yule, Cardiff Metropolitan University
Breast cancer is the most common cancer in the UK. It accounts for 15% of all new cases in the country, and about one in eight women will be diagnosed with it during their lifetime. In the NHS, breast cancer screening routinely includes a mammogram, which is essentially an X-ray of the breast.
But the future of this early test is at risk as the number of specialists able to read them declines. While this skills shortfall can’t be made up immediately, promising advances in artificial intelligence may be able to help.
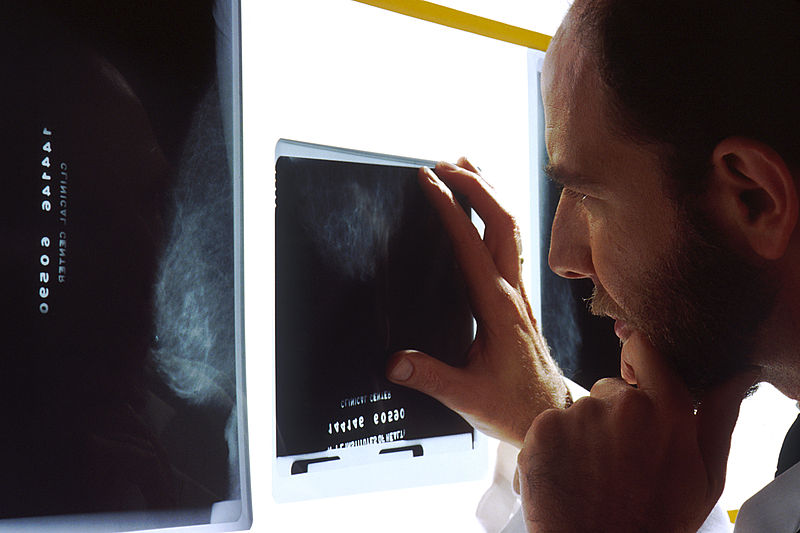
Interpreting a mammogram is a complex process normally performed by specially trained radiologists and radiographers. Their skills are vital to the early detection and diagnosis of this cancer. They visually scrutinise batches of mammograms in a session for signs of breast cancer.
But these signs are often ambiguous or hard to see. False negative rates – where cancers are incorrectly diagnosed or missed – are between 20 and 30% for mammography. These are either errors in perception or errors in interpretation, and can be attributed to the sensitivity or specificity of the reader.
It is widely believed that the key to developing the expertise needed to interpret mammograms is rigorous training, extensive practice and experience. And while researchers like myself are looking into training strategies and perceptual learning modules which can expedite the transition from novice reader to expert, others have been investigating how AI could be used to speed up diagnosis and improve its accuracy.
Machine diagnosis
As in countless other fields, the potential for AI algorithms to help with cancer diagnosis has not gone unrecognised. Along with breast cancer, researchers have been looking at how AI can improve the efficacy and efficiency of care for lung, brain and prostate cancer, in order to meet ever increasing diagnosis demands.
Even Google is looking at how AI can be used to diagnose cancer. The search giant has trained an algorithm to detect tumours which have metastasised, with a 99% success rate.
For breast cancer, the focus so far has been on how AI can help diagnose the disease from mammograms. Every mammogram is read by two specialists, which can lead to potential delays in diagnosis if there is a shortfall in expertise.
But researchers have been looking at introducing AI systems at the time of the screening. The idea is that it would support a specialist’s findings without waiting for the second opinion of another professional. This would reduce the waiting time and associated anxiety for the women who have been tested.
AI has already made substantial strides in cancer image recognition. In late 2018, researchers reported that one commercial system matched the accuracy of over 28,000 interpretations of screening mammograms by 101 radiologists. This means it achieved a cancer detection accuracy comparable to an expert radiologist.
In another study led by the same researcher, radiologists using an AI system for support showed an improved rate of improved breast cancer detection – rising from 83% to 86%. This research also found that using an AI system reduced the amount of time radiologists spent analysing the images on screen.
Fine tuning
But while the potential of AI has been welcomed by some radiologists, it has brought suspicion from others. And though other researchers have also found that AI is just as good at detecting breast cancers from mammograms as its human counterparts, this comes with the caveat that more fine tuning and software improvement is needed before it can be safely introduced into breast screening programmes.
Exciting as it may be to think that AI could be used to help detect such a prevalent cancer, specialist and public confidence needs to be taken into consideration before it can be introduced. Acceptance of the technology is vital so that patients and medical professionals know they are receiving the correct results.
As yet, there has been little research into the public perception of AI in breast cancer screening, but more general studies into AI and healthcare have found that 39% of people are willing to engage with artificial intelligence/robotics for healthcare. This rises to 55% for the 18- to 24-year-old demographic.
The AI systems are still in the research phase, with no firm plans to use it to diagnose patients in the UK yet. But these promising results show there is a tremendous opportunity for the delivery of radiology healthcare services, and ultimately the potential to detect more patients with breast and other cancers.
Helen Yule, PhD Researcher in Breast Radiology and Consultant Radiographer, Cardiff Metropolitan University
This article is republished from The Conversation under a Creative Commons license. Read the original article.