The heart and brain are two of the most critical organs in the human body. Working together, they make sure we stay alive and thrive.

By Kseniya Efremova ,Washington State Department of Health
What happens when a heart attack or stroke disrupts the normal functioning of these organs? In many instances, brain and heart tissue begin to die at an extremely fast pace. Studies show that up to two million brain cells can die every minute during a stroke.
The good news is that both stroke and heart attack are treatable. The faster you get treatment, the more likely you are to recover with limited to no disability — and Washington has a system in place to see that you do. You have a crucial job to do as well.
Why should I act FAST and call 9–1–1?
The longer you’re not getting blood to an area of your brain or heart, the more permanent damage is done. Also, in many situations, there’s a short time window for treatment. For most strokes, that window is three hours from the time symptoms start.
This is why it’s so important for you to call 9–1–1 at the first sign of stroke or heart attack. Calling 9–1–1 starts the system we’ve developed to get you to the right hospital in time to get treated. It’s called the Emergency Cardiac and Stroke System.
Why have an Emergency Cardiac and Stroke System?
A 2008 report showed that care, resources and outcomes for heart attack and stroke varied across the state. People having a heart attack or stroke were often taken to the hospital closest to them, only to be transferred to another hospital to provide needed treatment, resulting in unnecessary treatment delays. Washington needed a system to help get the right patient to the right facility in the right amount of time.
How does the system work?
On the prehospital (EMS) side, the Department of Health sets standard procedures that help EMS agencies assess whether a person is having a heart attack or stroke and decide which hospital to take the patient to.
Once the destination hospital is determined, EMS calls the hospital with a heads up that they’re bringing in a heart attack or stroke patient. The hospital calls in the appropriate medical team and gets everything ready for rapid assessment of the patient. Calling 9–1–1 saves time, which saves brain and heart tissue and improves chances of a good recovery.
In order for the system to work, EMS agencies have to know what cardiac and stroke capabilities hospitals have. Participating hospitals submit an application to the Department of Health, showing that their facility meets a certain level of cardiac or stroke care.
For example, to be categorized as a Level I stroke center, the hospital has to have a neurosurgeon available on site within 30 minutes of being notified of a stroke patient’s arrival. This service should be provided 24 hours a day, seven days a week.
A Level III stroke center, on the other hand, is not required to have a neurosurgeon, but must have a physician able to diagnose a stroke and begin appropriate care.
Whether a hospital is a Level I or a Level III, by working together and in conjunction with EMS, hospitals are able to make the most out of the resources available to them and ultimately, benefit the patient.
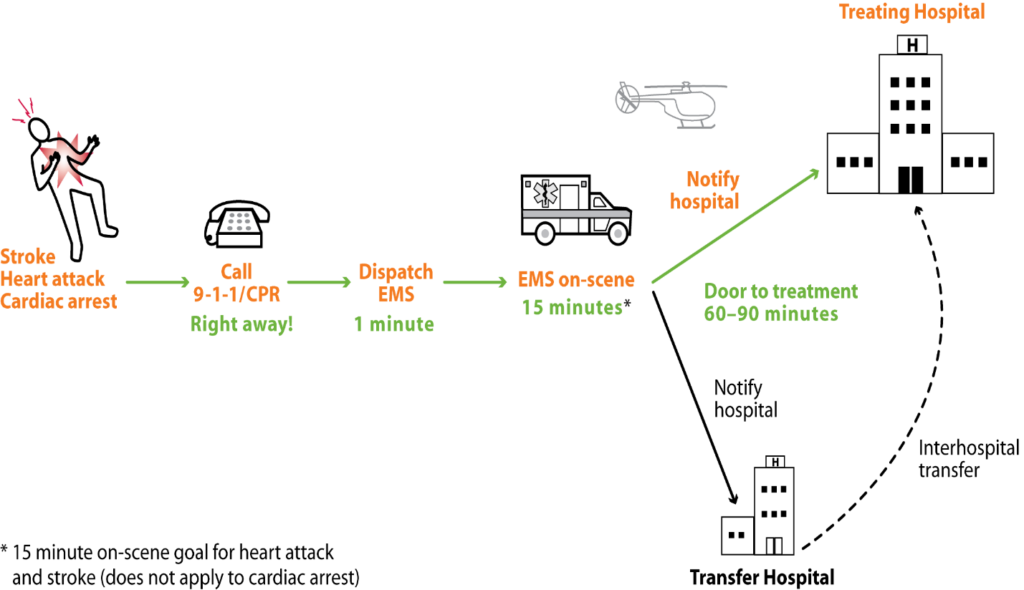
The following diagram helps explain how an organized system works to get patients to treatment less than 120 minutes after their symptoms begin:
What can I do to help?
You are the first step in the system! You can get treated in time or help someone else by knowing the symptoms of heart attack and stroke and by pledging to activate the system right away by calling 9–1–1 for medical emergencies. Together, we can save time and save lives!
Kseniya Efremova is a Stroke Program Specialist at the Washington State Department of Health.


