Judith Graham, Kaiser Health News
Close down group meals for seniors. Cancel social gatherings.
The directive, from the Illinois Department on Aging, sent shock waves through senior service organizations late last week.
Overnight, Area Agencies on Aging had to figure out how to help people in their homes instead of at sites where they mingle and get various types of assistance.
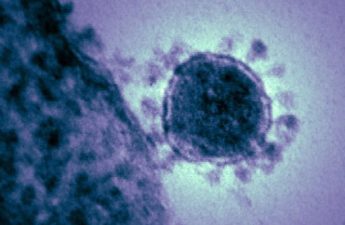
This is the new reality as the COVID-19 virus barrels into communities across America. Older adults — the demographic group most at risk of dying if they become ill ― are being warned against going out and risking contagion.
And programs that serve this population are struggling to ensure that seniors who live in the community, especially those who are sick and frail, aren’t neglected.
This vulnerable population far outstrips a group that has received more attention: older adults in nursing homes. In the U.S., only 1.4 million seniors reside in these institutions; by contrast, about 47 million older adults are aging in place. An additional 812,000 seniors make their homes at assisted living facilities.
While some of these seniors are relatively healthy, a significant portion of them are not. Outside of nursing homes, 15% of America’s 65-and-older population (more than 7 million seniors) is frail, a condition that greatly reduces their ability to cope with even minor medical setbacks.
Sixty percent have at least two chronic conditions, such as heart disease, lung disease or diabetes, that raise the chance that the coronavirus could kill them.
But the virus is far from the only threat older adults face. The specter of hunger and malnutrition looms, as sites serving group meals shut down and seniors are unable or afraid to go out and shop for groceries. An estimated 5.5 million older adults were considered “food insecure” — without consistent access to sufficient healthy food ― even before this crisis.
As the health care system becomes preoccupied with the new coronavirus, non-urgent doctors’ visits are being canceled. Older adults who otherwise might have had chronic illness checkups may now deteriorate at home, unnoticed. If they don’t go out, their mobility could become compromised — a risk for decline.
Furthermore, if older adults stop seeing people regularly, isolation and loneliness could set in, generating stress and undermining their ability to cope. And if paid companions and home health aides become ill, quarantined or unable to work because they need to care for children whose schools have closed, older adults could be left without needed care.
Yet government agencies have not issued detailed guidance about how to protect these at-risk seniors amid the threat of the COVID-19 virus.
“I’m very disappointed and surprised at the lack of focus by the CDC in specifically addressing the needs of these high-risk patients,” said Dr. Carla Perissinotto, associate chief for geriatrics clinical programs at the University of California-San Francisco, referring to the Centers for Disease Control and Protection.
In this vacuum, programs that serve vulnerable seniors are scrambling to adjust and minimize potential damage.
Meals on Wheels America CEO Ellie Hollander said “we have grave concerns” as senior centers and group dining sites serving hot meals to millions of at-risk older adults close. “The demand for home-delivered meals is going to increase exponentially,” she predicted.
That presents a host of challenges. How will transportation be arranged, and who will deliver the meals? About two-thirds of the volunteers that Meals on Wheels depends on are age 60 or older ― the age group now being told to limit contact with other people as much as possible.
In suburban Cook County just outside Chicago, AgeOptions, an Area Agency on Aging that serves 172,000 older adults, on Thursday shuttered 36 dining sites, 21 memory cafes for people with dementia and their caregivers, and programs at 30 libraries after the Illinois Department on Aging recommended that all such gatherings be suspended.
Older adults who depend on a hot breakfast, lunch or dinner “were met at their cars with packaged meals” and sent home instead of having a chance to sit with friends and socialize, said Diane Slezak, AgeOptions president. The agency is scrambling to figure out how to provide meals for pickup or bring them to people’s homes.
With Mather, another Illinois organization focused on seniors, AgeOptions plans to expand “Telephone Topics” — a call-in program featuring group discussions, lectures, meditation classes and live performances — for seniors now confined at home and at risk of social isolation.
In New York City, Mount Sinai at Home every day serves about 1,200 older adults who are homebound with serious illnesses and disabilities — an extraordinarily vulnerable group.
A major concern is what will happen to clients if home care workers become sick with the coronavirus, are quarantined or are unable to show up for work because they have to care for family members, said Dr. Linda DeCherrie, Mount Sinai at Home’s clinical director and a professor of geriatrics at Mount Sinai Health System.
With that in mind, DeCherrie and her colleagues are checking with every patient on the program’s roster, evaluating how much help the person is getting and asking whether they know someone ― a son or daughter, a friend, a neighbor — who could step in if aides become unavailable. “We want to have those names and contact information ready,” she said.
If caregivers aren’t available, these frail, homebound patients could deteriorate rapidly. “We don’t want to take them to the hospital, if at all possible,” DeCherrie said. “The hospitals are going to be full and we don’t want to expose them to that environment.”
In San Francisco, UCSF’s Care at Home program serves about 400 similarly vulnerable older adults. “Testing [for the coronavirus] is even more of a problem for people who are homebound,” said Perissinotto, who oversees the program. And adequate protective equipment ― gloves, gowns, masks, eye shields — is extremely difficult to find for home-based providers, Perissinotto said, a concern voiced by other experts as well.
To the extent possible, UCSF program staff are trying to do video visits so they can assess whether patients are symptomatic ― feverish or coughing — before going out to their homes. But some patients don’t have the technology that makes that possible or aren’t comfortable using it. And others, with cognitive impairments who don’t have family at home, may not be able to respond appropriately.
At UCSF’s general medicine clinic, nonessential medical visits have been canceled. “I have a lot of older patients with chronic pain or diabetes who otherwise would come in for three-month visits,” said Dr. Anna Chodos, a geriatrician and assistant professor of medicine who practices in the clinic. “Now, I’m talking to them over the phone.”
“I’m less worried about people who can answer the phone and report on what they’re doing,” she said. “But I have a lot of older patients who are living alone with mild dementia, serious hearing issues and mobility impairments who can’t work their phones.”