Public Health Insider, Public Health – Seattle & King County
The dramatic recent increase in COVID-19 cases in King County reflects a wide range of activities and settings where people may be getting exposed to the SARS-CoV-2 virus, the virus that causes COVID-19.
Instead of a few “hotspots,” COVID-19 risk is dispersed across homes, businesses, and other places where people gather.
Currently, with a case-rate above 380 cases per 100,000 residents – triple what it was in early October – the virus is widespread in King County.
It’s fair to assume at this time that exposure can happen anywhere you are around other people, especially indoors.
The most common reported sources of potential exposure in recent weeks are in households, in a variety of community or social activities and gatherings, and in workplaces.
A new report on outbreaks and exposure settings from Public Health—Seattle & King County describes settings where people may have become infected and finds the most common reported sources of potential exposure in recent weeks are in households, in a variety of community or social activities and gatherings, and in workplaces.
Examples of community and social activities include get-togethers with family and friends, birthday parties, house or dinner parties, larger celebrations such as weddings, activities at a place of worship or visiting food service establishments.
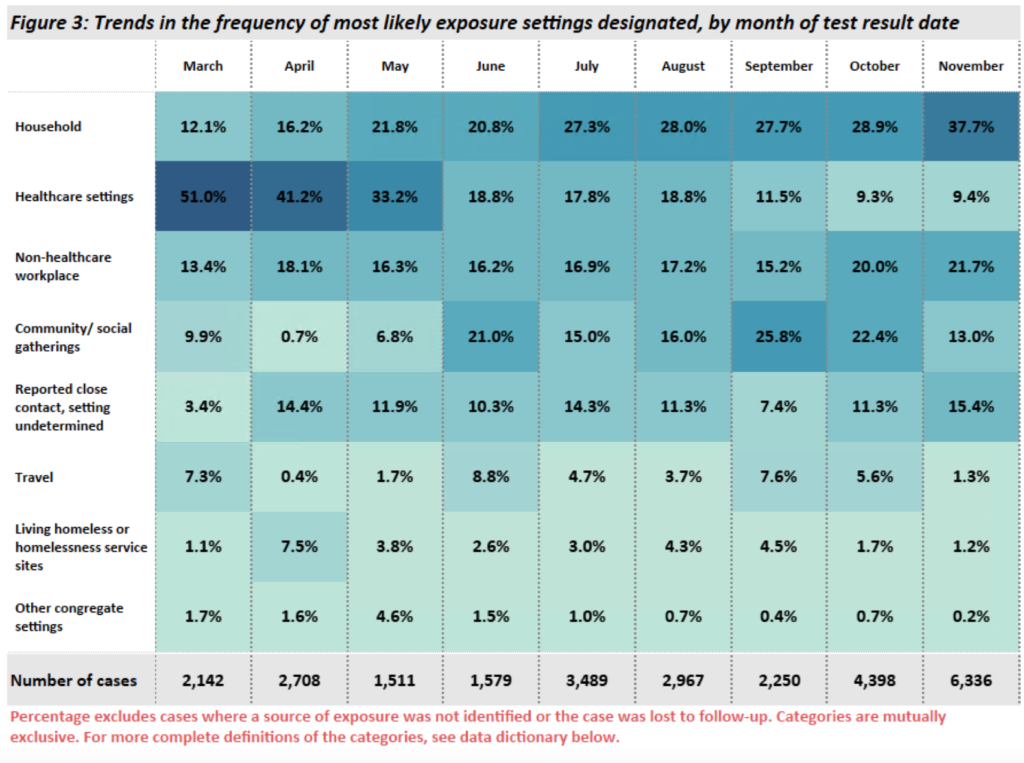
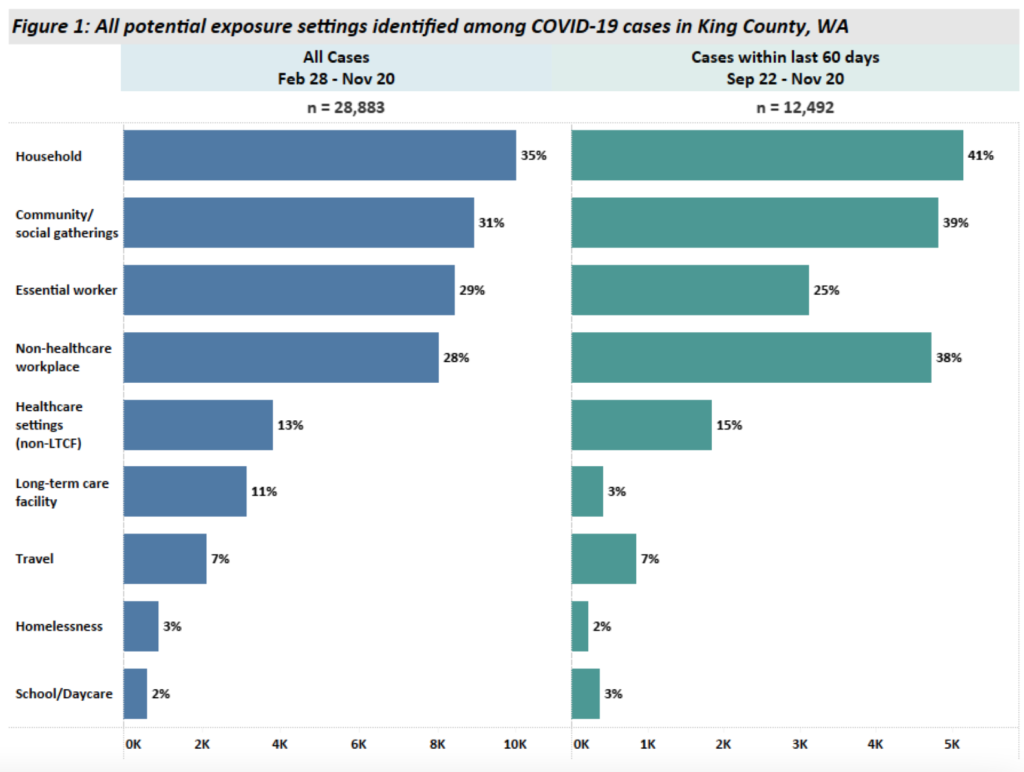
These activities, as well as out of state travel, have increased over the course of the pandemic while cases associated with long-term care and other healthcare facilities have decreased.
There are differences in potential sources of exposure by race and ethnicity, geography and age. In some of our most-impacted communities, particularly in south King County, workplaces are more frequently reported as a potential exposure setting.
This reflects that in some communities, people have fewer options to limit their exposure, like the option of working from home or isolating from others inside the home if they become ill.
When people who can limit their social exposure do so, they’re supporting essential workers and others who may not have a choice. More information on exposures by race/ethnicity and geography.
Types of places and activities where exposures are happening
When we asked people about where they have been outside of their household during their exposure period (two to 14 days prior to illness) social and community activities and gatherings top the list.
Over the last 60 days (from Sept. 22 to Nov. 20), 39% of cases reported they had spent time in community or social settings* where exposure to someone with COVID-19 was possible during the period just before they developed the infection.
Many people with COVID-19 have identified they were in more than one exposure setting that could pose a risk for COVID-19 transmission. For many cases, it’s not possible to know with certainty where transmission occurred.
Among the community settings, 24% of COVID-19 cases reported recent social events with friends or family; 15% visited food-service establishments; and 4% attended a place of worship.
In addition, 15% reported visiting, working, living, or being a patient in a healthcare; 7% traveled out of state or internationally; and, 2% were associated with homeless service sites or living homeless.
Contact inside a household (41%) and by working as an essential worker (25%) are the other leading pathways for potential exposures. Essential workers include healthcare workers, hospitality or service industry workers, and other essential workers.
Outbreaks and other exposure settings
Over the past 60 days, about 25% of all reported COVID-19 cases in King County can be linked to a known outbreak with two or more cases. Investigators from Public Health are routinely finding that community/social and household COVID-19 exposures typically occur when people have close contact in indoor spaces and are not wearing masks.
Since the start of the pandemic, Public Health has identified 836 outbreaks across the county. On average, eight cases were identified per outbreak (defined as two or more cases within 14 days among people in a common setting) although it’s not always possible to identify and test all exposed people.
Earlier in the pandemic, most outbreaks were in long-term care facilities and homeless services sites. In the past two months, the largest numbers of identified outbreaks are in manufacturing and construction workplaces (53 outbreaks; average of 5 cases per outbreak from Feb. to present) and in food service establishments (40 outbreaks; average of 3 cases per outbreak from Feb. to present).
To interpret what this data tells us, we asked Health Officer Dr. Jeff Duchin the following questions:
Q: If I want to get out of the house, what settings are safest and which should I be avoiding?
A: Anyone – even your family, friends and co-workers – can spread COVID-19 before they look or feel ill. This means we can’t tell if someone has COVID-19 by looking at them or by how they feel. That’s why we should all expect COVID-19 where we don’t expect it. There are places that are especially high risk, like crowded indoor locations and places with poor ventilation. An important take-away from the report is that infections are happening at a wide variety of locations. In addition to essential workplaces, many cases are associated with social gatherings that are not essential, like get-togethers with family and friends, dinners, parties, and other celebrations.
It’s also important to remember that according to the Centers for Disease Control and Prevention there is growing evidence that droplets and airborne particles containing the virus that causes COVID-19 can remain suspended in the air and be breathed in by others, and can travel distances beyond 6 feet (for example, during choir practice, in restaurants, or in fitness classes). In general, indoor environments without good ventilation increase this risk.
Q: If homes are one of the most common places people are exposed to coronavirus infections, the virus still had to get into those homes, right? What do we know about the source of exposure within a household?
A: COVID-19 is introduced into homes through exposure to one or more household members who become infected in the community, such as in the workplace, or through social activities. We know that 29% of all cases are among essential workers. Essential workers may transmit the virus to those they live with. For this reason, it’s important that workplaces follow current COVID-19 safety and prevention requirements such as screening workers for symptoms, keeping people separated as much as possible, wearing masks, and improving ventilation. COVID-19 can also spread if people let down their guard when gathering in break rooms at work, socialize with co-workers outside of work, or commute together, especially if precautions like mask use and distancing are not taken.
Another important pathway is social and community gatherings. If one household member goes out and socializes, even with a small group of friends, or participates in group gatherings, they may bring the virus into the home before they are symptomatic or are aware they were exposed. By limiting activities and contact with others outside the home, wearing a face covering when with others, avoiding crowded indoor spaces, and keeping contacts brief and with 6 feet or more of physical distance, you are reducing the risk for yourself as well as anyone you live with.
Once someone is infected within a household, it can be difficult to prevent spread, but there are supports for people who cannot safely isolate at home. Learn more about how to care for someone who is ill with COVID-19. People who are exposed to someone with COVID-19 should quarantine for 14 days after the last exposure, and be tested – especially if symptoms develop.
Q: What does the report tell us about the role of food service establishments in the spread of COVID-19?
A: Restaurants accounted for the second highest number of non-healthcare-facility outbreaks reported to us since the pandemic began (83 since the start of the pandemic and 40 in the last 60 days). From our case and contact tracing interviews, 15% of cases in the past 60 days reported visiting a food-service establishment/restaurant.
It’s difficult to accurately estimate the precise burden of transmission associated with a business or retail setting like a restaurant or other food service establishment for several reasons. At these businesses, there is no guest or participant list allowing follow up with potentially exposed persons as there is in other settings like private social events or other community gatherings. Also, information from interviews is often incomplete making it hard to recognize common exposures among people. And finally, people may be exposed at more than one setting in the community and unless linked to an outbreak, we don’t often know with certainty which exposure led to the infection.
Independent of our report, a robust evidence base has established that COVID-19 spreads through small particles emitted when people breathe and talk. Some of these particles may remain suspended in the air and can cause infection at distances greater than 6 feet. Risk is increased indoors and with the duration of exposure, proximity to others, when masks are not worn, and with activities that increase the exhalation of virus including loud talking. If you have to remove your mask to eat or drink, that increases the risk. Since the beginning of the pandemic, multiple reports of clusters and outbreaks of COVID-19 associated with patronage at restaurants and bars have been published in the scientific literature.
For these reasons, indoor seating at restaurants and bars is widely considered to be a high-risk activity by public health and medical experts, including the Infectious Diseases Society of America, the Centers for Disease Control and Prevention (CDC) and others.
Q: Public Health is investigating hundreds of potential outbreaks. Are there commonalities you are seeing among the outbreak investigations?
A: In general, we are seeing an increasing number of reports from a range of workplaces such as manufacturing, food production and food service, retail and construction. We’ve also had recent outbreaks associated with faith-based organizations, and we continue to see outbreaks in a variety of healthcare settings. While people may be careful during their work time, including wearing PPE, COVID-19 is highly contagious and can still spread in some environments when precautions are difficult to adhere to. We also know that people come in contact with others in the community and socialize during breaks, outside of work and while commuting to work. These are times when it’s very important for people to keep wearing their masks, washing hands, keeping at least six feet of distance from one-another and increasing ventilation as much as possible.
Q: What does the data tell us about how public health efforts can control the spread of the virus?
A: We know prevention can really work as evidenced by the decline in cases and outbreaks in response to our community efforts during the spring. And in long term care facilities and healthcare settings, recent outbreaks have been smaller thanks to improved infection control measures. However, overall levels of COVID-19 transmission and outbreaks are increasing, and I am extremely concerned about rising case numbers and hospitalizations, the impacts on our healthcare system, and the disproportionate health outcomes we are seeing by race and ethnicity.
Based on the success of the measures that led to the suppression of our outbreak last spring, we know what we need to do to reduce the spread of the virus. We all need to limit our activities and social contacts outside the home and take all the other steps needed to prevent the spread of COVID-19 including wearing face masks, making any necessary contacts with others outside the home brief and with as much distance as possible, avoiding crowded indoor spaces, improving indoor ventilation, and remembering good hand hygiene.
Our communities are immensely resourceful and resilient. However, the health disparities we see during COVID-19 are based on ongoing inequities, and the disparities get exacerbated during health emergencies. We need to continue to partner with communities to identify barriers to health and develop supports that can have a meaningful impact in reducing the harmful impacts of the virus.
Q: What do you want to be sure people understand about the data and its limitations before they draw conclusions?
A: In addition to the limitations discussed above related to food service establishments, there are a few others to be aware of. First of all, it’s likely that for every case we hear about, there are several more cases that do not get diagnosed and reported. Likewise, for outbreaks, the data likely represents just the tip of the iceberg. While hospitals and restaurants are required to notify Public Health of outbreaks, we rely on businesses, schools and other organizations to voluntarily let us know when they suspect two or more cases. For these reasons we can’t say that the number of outbreaks we become aware of or their size represents the entire picture of what is actually happening in the community.
Secondly, because of the way COVID-19 spreads, it’s not usually possible to determine with certainty from our case investigations where individuals acquired COVID-19 in the community. It can be difficult for people to recall all the many places they may have been several days prior to testing positive. For example, consider how difficult it would be to determine where someone acquired the flu during a typical flu season.
The data that we do have provides valuable, although incomplete, information about the types of settings and activities where COVID-19 is being transmitted in King County. This information highlights important actions we can take to reduce the risk from COVID-19 to individuals and their household members and to decrease the spread of COVID-19 in our community.
* Definition of cases designated as community/social gatherings: Cases involved in socializing and visiting with family and friends, going to parties or celebrations (weddings, graduations events) and large social or public events or gatherings. This category also includes cases at colleges/universities, places of worship, visiting restaurant/bars or other food service establishments, and retail shopping.
Originally posted November 25, 2020


