By Christine Vestal, Stateline
The federal Centers for Disease Control and Prevention last month proposed new guidelines that would ease restrictions on prescription opioids, but states might balk at lifting limits on painkillers that have fueled the nation’s deadly overdose epidemic.
The proposed recommendations aim to give millions of Americans suffering intractable and chronic pain better access to the opioid painkillers their doctors say they need. At the same time, the proposed guidelines caution against starting any new patients on the highly addictive painkillers unless nothing else works.
For the eased guidelines to have their intended effect, states would need to amend or repeal existing statutes that limit opioid prescriptions to three to seven days and set ceilings on the daily dose doctors can prescribe.
But both physicians and addiction experts, who typically do not agree on the opioid prescribing issue, predict that few governors or lawmakers will be eager to loosen restrictions that were difficult to put in place, especially with the overdose epidemic still raging.
“Relaxing those regulations now would wreak havoc on states. They won’t know what to do,” said Dr. Gary Franklin, who as medical director of Washington state’s workers’ compensation agency was instrumental in enacting his state’s restrictions on opioid painkillers in 2017.
“We’ve made quite a dent in prescription painkiller use,” Franklin said. “But we’ve still got a lot of work to do.”
Although the American Medical Association and groups representing pain patients and their doctors would like to see state prescribing regulations repealed, they say they don’t expect that to happen overnight.
That would be a “heavy lift,” said Dr. Bobby Mukkamala, chair of the AMA Board of Trustees, which has been advocating for greater physician latitude in pain management since the CDC’s first set of guidelines were issued in 2016.
“The old language was a real problem,” Mukkamala said. “When it got down to states and individual insurers and health systems it became dogma, it became gospel. It really left patients in a bad position.”
Those initial CDC guidelines recommended that doctors limit initial prescriptions of opioid painkillers to no more than a week and set a maximum daily dose that is roughly equal to 90 mg of morphine.
Rather than limiting the number and strength of painkillers physicians can prescribe, the new guidelines would give doctors wide discretion to weigh the benefits of pain relief and improved physical function against the known risks of opioid painkillers.
Dr. Andrew Kolodny, senior scientist at Brandeis University’s Heller School of Public Policy, has long supported tighter restrictions on opioid painkiller prescribers. He praised the thoroughness of the CDC’s research review in its 211-page proposed guidelines.
But, he said, “the evidence is not congruent with its recommendations, which is all most prescribers will ever read. That’s what will be disseminated in one-page flyers.”
CDC Changes
The CDC put the 2016 guidelines in place to curb what was seen as massive overprescribing of highly addictive pain medicine. The guidelines, combined with state limits, medical board licensing restrictions and growing public awareness of the dangers of opioid painkillers, led to a sharp decline in U.S. opioid painkiller use, according to the CDC.
Since its peak in 2012, the rate of U.S. opioid dispensing dropped from 81 prescriptions per 100 people to 43 per 100 in 2020, with wide variations among states.
But in the process, millions of pain patients encountered multiple barriers to finding needed relief, according to the AMA and numerous pain experts and advocates for people with pain.
The CDC’s latest guidelines still stress that doctors should recommend non-opioid pain solutions such as ibuprofen, physical therapy and acupuncture before prescribing opioids, to reduce the risk of addiction and overdose. But they don’t recommend any set limits.
The CDC is seeking comments on the proposed guidelines through April 11, with a final document expected later this year.
“Millions of Americans experience pain each day, including approximately one in five who are living with chronic pain, and these patients deserve access to safe and effective pain care,” the acting director of the CDC’s National Center for Injury Prevention and Control, Christopher M. Jones, wrote Stateline in an email.
Asked whether the relaxed guidelines might impede efforts to quell the nation’s opioid epidemic, Jones noted that the vast majority of overdose deaths now involve illicit drugs such as fentanyl, methamphetamine and cocaine.
“We’ve learned that there is great variation in the practice of pain care and the experience of patients living with pain, and we recognize the harms that have resulted from misapplication of the 2016 guideline,” Jones wrote. “This update provides the opportunity to refine and improve the recommendations based on the latest science and the lived experiences of patients and providers.”
State Laws
In 2016, when the CDC’s landmark guidelines were published, state policymakers already were devising ways to protect the public from falling prey to what they saw as overprescribing of deadly opioid painkillers.
In addition to their own restrictions on opioid prescribing, most states began using prescription drug monitoring computer systems to enforce those rules and deter patients from doctor shopping to obtain more drugs.
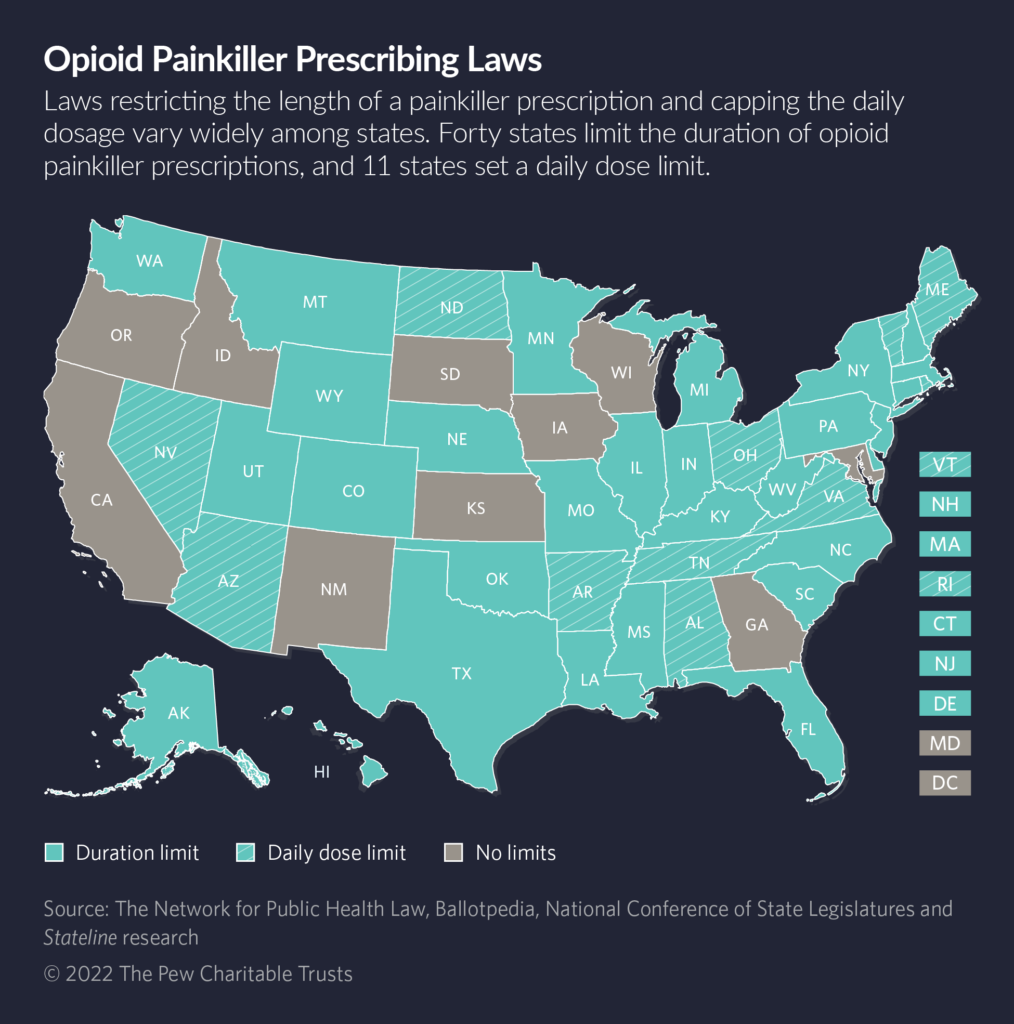
Massachusetts in 2016 became the first state to enact a law limiting the length of opioid painkiller prescriptions. As of this month, 40 states have laws on the books limiting the length of initial opioid prescriptions, and 11 states have laws capping the daily allowable dose.
But by 2019, the CDC and the U.S. Food and Drug Administration were warning prescribers that abruptly cutting off high-dose patients or tapering their doses too rapidly could cause withdrawal symptoms and even suicide.
In its new guidelines, the CDC stresses that physicians should never abandon patients who seek higher doses or longer use of painkillers than the existing recommendations. Some policies have gone beyond the 2016 recommendations, the agency wrote in its draft guidelines, contributing to “patient harm, including untreated and undertreated pain, serious withdrawal symptoms, worsening pain outcomes, psychological distress, overdose, and suicidal ideation and behavior.”
As a result, a few states have modified their opioid prescribing statutes over the past six years, allowing exceptions to the rules and extending the duration of prescriptions. Rhode Island, for example, enacted a law last year allowing doctors who treat patients with intractable or chronic pain to prescribe opioids and other controlled substances without regard to the CDC’s guidelines.
“There is no denying that we are still grappling with the severity of the opioid crisis and the pandemic has only made this matter worse, but we also cannot forget that to some, this medication allows them to function in their daily lives due to extreme chronic pain,” Rhode Island state Sen. Valarie Lawson, a Democratic co-sponsor of the bill, said in a statement following its passage.
But most states have left their original prescribing restrictions intact. North Dakota last year added both a seven-day limit on opioid prescribing and a 90 mg morphine equivalent cap on daily doses for patients treated by physicians under the state’s workers’ compensation program. That sprang from concern that too many workers were relying on high doses of painkillers that put them at risk of addiction and overdose.
Corey Davis, a deputy director at the Network for Public Health Law, which tracks the issue, said he doubted many states would rush out and change their prescribing laws and regulations because of the CDC’s new guidelines.
“Many states took the CDC’s thresholds and turned them into strict limits that were misconstrued or overread by providers who didn’t want to get in trouble and didn’t want to be hassled,” Davis said.
“My hope,” he said, “is that those states will take the opportunity to revisit those strict limits and turn them into more holistic, nuanced policies that address the complexities of addiction and pain management.”


