Adam Taylor, Lancaster University
American journalist Grant Wahl, who died while reporting on a match during the 2022 Qatar World Cup, is said to have suffered from a ruptured aortic aneurysm. This happens when bulging in the aorta (the main blood vessel that supplies oxygenated blood from the heart to the rest of the body) ruptures. Although the exact aneurysm Grant suffered is relatively uncommon, it is very dangerous if not caught in an early stage when it can be managed.
Our blood vessels fall into three main categories: arteries, capillaries and veins. The arteries take oxygenated blood from the heart and deliver it throughout the body, running through capillaries in the tissues and then passing into veins to return it to the heart.
While aneurysms can occur in any blood vessel, they most commonly happen in major arteries (such as the aorta) or blood vessels in the brain. The aorta is the largest of the more than 60,000 miles of blood vessels that run through our body. It receives the highest-pressure blood, which is freshly ejected from the heart as it beats.
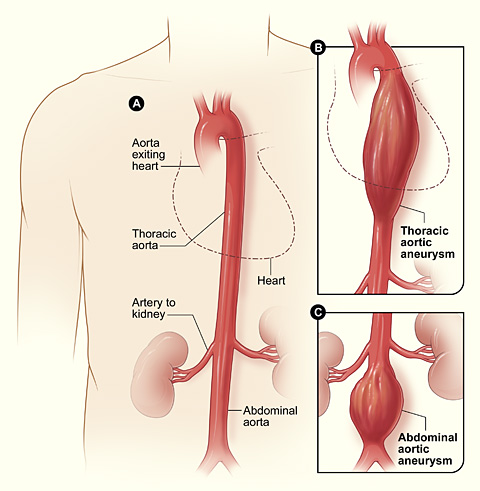
The aorta runs through the thorax and the abdomen. As such, there are two main types of aortic aneurysms. Thoracic aortic aneurysms – the location of the aneurysm Wahl had – form in the chest area. These are rare, being seen in only 6-10 people per 100,000. They can form anywhere along the aorta in the chest. In Wahl’s case, it was on the first part of the aorta, which is also called an ascending aortic aneurysm.
Abdominal aortic aneurysms occur in the abdomen. These are much more common, affecting between 4% and 13% of men and 6% of women over the age of 65.
Both types of aortic aneurysm are associated with atherosclerosis, a condition that hardens and narrows the arteries. This damages and alters the lining of the blood vessel, causing the artery to bulge and the blood vessel wall to weaken. If this bulge isn’t treated, it can then tear through the innermost layer of the blood vessel or rupture the artery entirely.
Risk factors
There are several common risk factors for developing either type of aortic aneurysm.
Men are three to four times more likely to have an abdominal aortic aneurysm and two to three times more likely to have a thoracic aortic aneurysm. However, women are twice as likely to have a brain aneurysm and are much more likely to die from a thoracic aortic aneurysm as the disease progression is much quicker.
Age is another big factor, with both thoracic and abdominal aortic aneurysms being most common in men over 65 years of age. The likelihood of developing an abdominal one also increases between 2% and 4% every decade after 65.
White people have a greater risk of aortic aneurysm – though black people are more likely to experience complications after having an aortic aneurysm repaired. A family history of aneurysm also increases the likelihood of having one. If your parent or sibling had an abdominal aortic aneurysm, your risk increases fourfold, whereas 20% of people with a thoracic aortic aneurysm, will have a first-degree family member with the condition.
People with the genetic condition Marfan syndrome – which affects their connective tissues – have an increased risk of aneurysms due to the blood vessel walls being weak.
Cocaine use is also associated with an increased risk, particularly in younger people with no other risk factors. It’s believed cocaine use causes severe hypertension and weakens arterial walls.
Smoking is the biggest risk factor for abdominal aortic aneurysms. This is because the nicotine in tobacco contributes to atherosclerosis.
Symptoms and treatment
Aneurysms are usually symptomless. But if abdominal aortic aneurysms become large enough, a doctor may be able to feel it “pulsating” through the abdominal wall. Abdominal pain and back pain may also occur, usually before rupture.
Thoracic aneurysms are much more difficult to diagnose, and they cannot be felt by a doctor. They may cause persistent cough, chest and neck pain, as well as difficulty breathing. These become significantly worse with rupture.
Abdominal aortic aneurysms are usually identified using an ultrasound, while thoracic aneurysms require an X-ray, CT or MRI scan or an ECG. This will only be done if a doctor suspects you have an aneurysm, though in some countries men over the age of 65 are offered an ultrasound as part of screening programmes for abdominal aortic aneurysms.
The diameter of a normal aorta is between 2cm and 3cm. To be considered aneurysmal, the diameter of the vessel must be 1.5 times its normal size. People with small and medium aneurysms (between 3cm and 5.4cm) may not need surgery and can slow the growth of their aneurysm by making lifestyle changes – such as stopping smoking, exercising and eating a healthy diet.
But aneurysms bigger than 5.5cm carry a high risk of rupture, so surgery will be recommended to repair it. If an aneurysm this size ruptures, there is a 90% chance of death if it happens outside of a hospital. The surgery can be done using two methods.
Open surgery involves making a large incision in the abdomen or chest wall. An artificial graft made of synthetic material, such as polyester, is put in where the damaged aorta is. More recently, there has been a move to a less invasive surgery called endovascular aneurysm repair. This sees a graft fed in through an artery in your groin and then moved into place to repair the aorta. This can only be done if the patient’s blood vessels are healthy enough.
Aneurysms are extremely dangerous if not caught early. The good news is their prevalence in men over 65 is falling – possibly due in part to healthier lifestyles and fewer people smoking. But it will be important to continue screening programmes, and possibly even begin screening men at younger ages to prevent tragedies like what happened to Grant Wahl.
Adam Taylor, Professor and Director of the Clinical Anatomy Learning Centre, Lancaster University
This article is republished from The Conversation under a Creative Commons license.
Read the original article.


