Three years on, the COVID pandemic may never end – but the public health impact is becoming more manageable
Michael Head, University of Southampton
Three years ago, on March 11 2020, World Health Organization (WHO) director-general Tedros Adhanom Ghebreyesus first formally described COVID-19 as a pandemic.
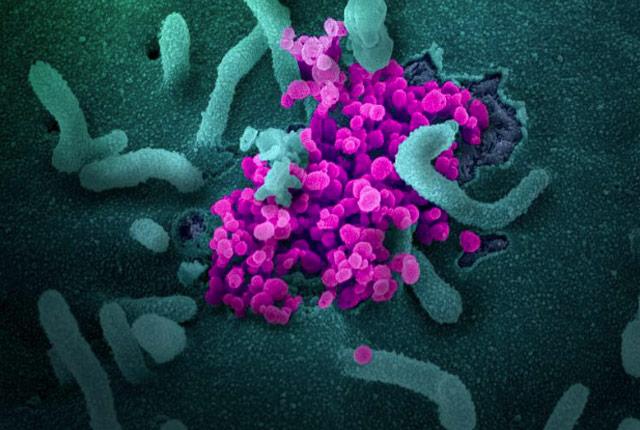
The impact of the pandemic on all aspects of society has been enormous, but we’ve come a long way since March 2020. The toll of this novel coronavirus has been blunted thanks to responses across science, healthcare and public health.
At this point, it’s not unreasonable to wonder when the pandemic will be over. But the WHO continues to regard COVID as a pandemic. Let’s take a look back at how we got here and explore where we might be heading.
First, what actually is a pandemic?
The term “pandemic” can have slightly different definitions depending on where you look. However, perhaps the most common use of the term applies to an emerging threat that is spreading across multiple countries: “an epidemic occurring worldwide”.
Essentially, a pandemic is one level above a public health emergency of international concern (PHEIC). The WHO declared COVID a PHEIC (pronounced “fake”) on January 30, 2020.
A PHEIC, as defined in the International Health Regulations, is “an extraordinary event” where there’s a risk of international disease spread, and which might require a coordinated international response. Previous examples include the 2014 West Africa Ebola outbreak, the 2016 emergence of the Zika virus, and the 2022 mpox (monkeypox) outbreak.
Interestingly though, in contrast to a PHEIC, the WHO doesn’t have the power to officially declare the start or end of a pandemic. This is because the term is not a category in the International Health Regulations, an important legal instrument. However, the WHO’s labelling of COVID as a pandemic carries a lot of weight and it has become widely regarded as such.
Emergency committees may decide what constitutes a pandemic versus a PHEIC based on factors including the severity of the disease, its mode of transmission, and its impact on nations.
A transition point
On January 30 2023, exactly three years after the PHEIC declaration, the WHO released a new statement indicating that COVID should still be regarded as a PHEIC, but noting that “the COVID-19 pandemic is probably at a transition point”. This recognises the fact that high levels of immunity to COVID are now limiting its impact.
The transition point refers to the de-escalation of COVID as a PHEIC, which some have speculated may happen in April. Indeed, Adhanom Ghebreyesus said in December 2022 that the WHO was hopeful that “we will be able to say that COVID-19 is no longer a global health emergency” at in some point in 2023.
This shift would lessen available funding and international co-ordination. This must be balanced alongside appropriate action that considers the continuing burden of COVID, recognising that each country will be at a different stage of their pandemic management.
In that statement, there’s continued reference to an ongoing “pandemic”. This is not unreasonable, as COVID really continues to meet any commonly used definition. There is, and will be for the foreseeable future, sustained transmission across multiple countries alongside a significant burden of hospitalisations and deaths. Therefore, we may end up in the situation where there is technically an ongoing pandemic despite a declared end to the PHEIC. Such are the difficulties in defining the different stages of a global crisis.
There are still around 150,000 confirmed cases globally each day, with many more not being recorded as real-time data management is relaxed across most countries.
Nations such as China have reported numerous outbreaks across late 2022 and early 2023, with significant impact on their health services. Long COVID will continue to affect millions of people.
The extensive misinformation from influential anti-vaccination activists continues to be a problem, with the WHO citing the need to “address the infodemic”.
So despite the incredible success of the COVID vaccines, and other public health efforts to bring outbreaks largely under control, the pandemic isn’t yet past tense. We are, however, moving out of the emergency response phase.
How did other pandemics end?
There was a declared and definitive end to the 2009–2010 swine flu pandemic. This was a little easier due to the seasonal influenza patterns, something we don’t see with COVID.
Although real-time surveillance would have been limited, there were also relatively clear ends to the influenza pandemics of 1918–1919 and 1957–1958.
The precise ends to pandemics further back in history such as the Black Death in the 14th century and the large-scale outbreak of smallpox in the 16th century are unclear, but ultimately defined from retrospective reporting in the history books, rather than scientific committees.
It’s somewhat easier to declare a new PHEIC or define the start of pandemic, compared with the end. If the outbreak simply does not end, then declaring a time point at which “it’s over” is understandably tricky.
As the WHO indicate in their recent statement, there needs to be a continued focus on COVID beyond any defined end of the public health emergency. This focus must remain even as countries consider how to mainstream their disease control into more routine public health and health service infrastructure.
The COVID pandemic may never be over. However, the public health threat of this virus should continue to decline. The need to learn lessons from this pandemic ahead of the inevitable next time is essential. History has shown us that infectious diseases have the capacity to evolve and emerge unpredictably. The next pandemic may be just around the corner – and we don’t know which corner.
Michael Head, Senior Research Fellow in Global Health, University of Southampton
This article is republished from The Conversation under a Creative Commons license.
Read the original article.


