Category: Health Policy
States struggle to help patients navigate insurance hurdle known as ‘step therapy’
Millions of Americans have experienced similar frustrations under protocols known as step therapy, or fail-first policies. Insurance companies, and the pharmacy benefit management companies that handle prescriptions for them, often refuse to cover a specific drug until after the patient has tried cheaper alternatives. Insurers argue that step therapy — taking drug treatment one step a time — prevents wasteful spending by directing patients to less expensive, but still effective, treatments.
Arizona’s now-repealed abortion ban serves as a cautionary tale for reproductive health care across the US
Medical students are less inclined to enter the specialty and more likely to avoid training positions, employment or both in states with restrictive or near-total bans. These states also have difficulty retaining existing OB-GYNs.
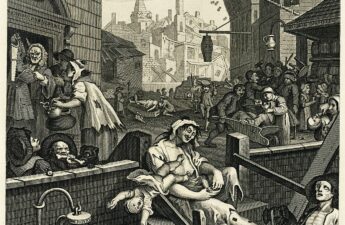
Future pandemics will have the same human causes as ancient outbreaks
Lessons from anthropology can help prevent them
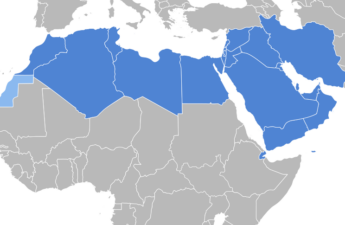
Census change will lead to more data on health of Middle Eastern, North African people in US
For decades, U.S. residents with heritage from the Middle East and North Africa, which is known internationally as the MENA region, have been classified by the government as white. The grouping masked differences in income, health, housing and other important markers.
Oregon’s Drug Decriminalization Aimed to Make Cops a Gateway to Rehab, Not Jail. State Leaders Failed to Make It Work.
Ballot Measure 110, approved by voters in 2020, created a new role for law enforcement in Oregon. While there’s evidence people living with addiction in the state are increasingly finding their way into treatment, the failure to turn police encounters into successful on-ramps to rehab has been cited by critics as prime evidence the measure isn’t working. Oregon lawmakers, noting an ongoing rise in overdose deaths, are now looking to restore jail time for drug possession.
But Oregon’s political leaders themselves played central roles in failing to deliver on the potential for law enforcement to connect people with lifesaving services under the new measure, documents and interviews with a wide array of people involved in the system indicate.
Governments can erase your medical debt for pennies on the dollar — and some are
Medical debt is the leading cause of bankruptcies in the United States, and more than 2 in 5 American adults have some. Some states and cities will use federal money to forgive millions of dollars of their residents’ medical debt.
Viewpoint: Restricting Obese Women From IVF Is Discriminatory
Fertility clinics bar women with obesity from their services, despite the lack of medical evidence for doing so.
10 Medicaid holdout states scramble to improve health coverage
The Republican-led states that have refused to expand Medicaid are trying a variety of strategies to save struggling hospitals and cover more people without full expansion, which was one of the key provisions of the Affordable Care Act.
Insurers often shortchange mental health care coverage, despite a federal law
The Biden administration is pushing insurers and state regulators to improve mental health care coverage. The move comes as overdose deaths rise and youth mental health problems grow more rampant, disproportionately affecting communities of color. Inflation and a shortage of mental health care providers, including psychiatrists and specialists who treat adolescents, further hinder access to care.
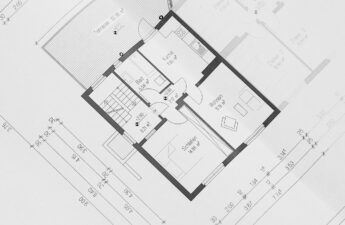
How Washington state is treating housing as health care
pple Health and Homes is a multi-agency state program launched last year that focuses on providing housing to people with health and behavioral health challenges. What’s unique is that the program taps Medicaid dollars to pay for housing subsidies, tenant services and more.
Some states back hospital mergers despite record of service cuts, price hikes
In much of the country, a single hospital system now accounts for most hospital admissions.
Book Review: Two Critiques of America’s Ailing Health Care System
Two recent books explore a truth that is obvious to nearly everyone who works in health care and surprising to almost everyone else: Through no fault of their own, doctors often don’t know what they are doing and, even when they do, America’s patchwork way of paying for health care may prevent them from doing it.
Act expands access to opioid use disorder treatment
Previously, providers were required to complete training and apply for a waiver from the Drug Enforcement Administration (DEA) to prescribe buprenorphine. Now, those with a current DEA registration that includes Schedule III authority can prescribe it.
How the Mixed Messaging of Vaccine Skeptics Sows Seeds of Doubt
By Darius TahirKaiser Health News It was a late-spring House of Representatives hearing, where members of Congress and attendees hoped to learn lessons from the pandemic. Witness Marty Makary made a plea. “I want to thank you for your attempts…
Why Finland is the happiest country in the world – an expert explains
Finland comes out top, followed by Denmark and Iceland. Just why Finns are happier than others comes down to a number of factors including lower income inequality (most importantly, the difference between the highest paid and the lowest paid), high social support, freedom to make decisions, and low levels of corruption.