Sara Sawyer, University of Colorado Boulder; Emma Worden-Sapper, University of Colorado Boulder, and Sharon Wu, University of Colorado Boulder
An outbreak of H5N1 avian influenza that started in 2021 has become the largest bird flu outbreak in history, both in the U.S. and worldwide. In the U.S. the virus has led to the destruction of millions of commercially raised chickens, turkeys, ducks and geese, and has killed thousands of wild birds.
Many virologists are concerned that this virus could spill over to humans and cause a new human pandemic. University of Colorado Boulder virologists Sara Sawyer, Emma Worden-Sapper and Sharon Wu summarize the compelling story of H5N1 and why scientists are closely watching the outbreak.
1. Is this virus a serious threat to humans?
H5N1 is a specific type of influenza virus, predominantly harbored by birds, that was first detected on a goose farm in China in 1996. Recently it has begun infecting an exploding diversity of bird and mammalian species around the globe.
The virus is highly pathogenic to birds, meaning that infections often cause extreme symptoms, including death. But its impact on humans is complicated. There have been relatively few human infections detected – fewer than 900 documented globally over several decades – but about half of those infected individuals have died.
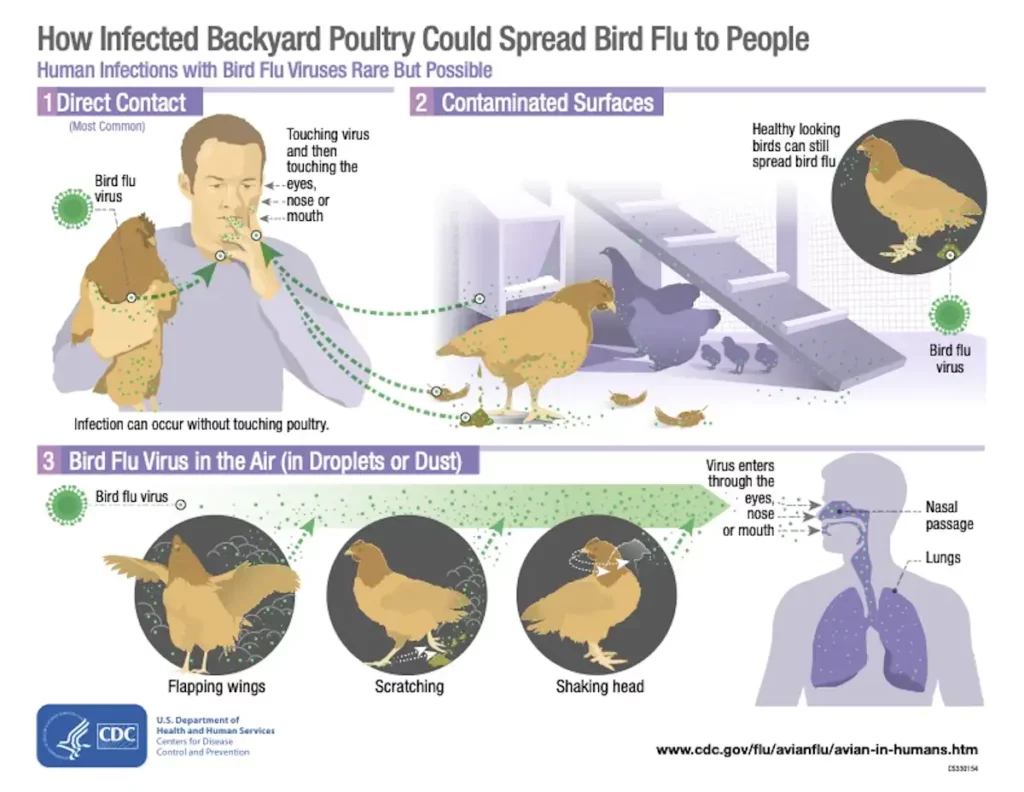
The good news about H5N1 for humans is that it currently doesn’t spread well between people. Most people who have contracted H5N1 have gotten it directly from interacting with infected poultry – specifically chickens, turkeys, ducks and geese, which often are raised in close quarters on large commercial farms.
There are only a small handful of examples of human-to-human spread. Because H5N1 doesn’t spread well between people, and because direct infection of humans by infected birds is still relatively rare, H5N1 has not yet erupted into a human epidemic or pandemic.
2. Why is this outbreak suddenly getting so much attention?
The first reason that so much attention is being paid to bird flu right now is that currently H5N1 is causing the largest “bird pandemic” ever recorded. A certain viral variant that arose in 2020, called H5N1 2.3.4.4b, is driving this outbreak.
In agricultural poultry flocks, if a few birds test positive for H5N1, the whole flock is killed regardless of symptoms or infection status. Higher prices for eggs and poultry meat in the U.S. are one result. The Biden administration is considering vaccinating farmed poultry flocks, but the logistics could be quite complicated.
The second reason for increased attention is that H5N1 is now infecting more bird and mammalian species than ever before. The virus has been detected in a broad array of wild birds and in diverse mammals, including badgers, black bears, bobcats, coyotes, ferrets, fisher cats, foxes, leopards, opossums, pigs, skunks and sea lions.
As H5N1 infects more species, it also increases its geographical range and produces more viral variants that could have new biological properties.
The third and most worrisome reason that this virus is getting so much press is that H5N1 now seems to be transmitting well between individuals of at least one mammalian species. In late 2022, mammal-to-mammal spread occurred in Spain in farmed minks. H5N1 spread very efficiently between the minks and caused clinical signs of illness and death in the mink populations where it was detected.
Sea lions in Peru are also succumbing to H5N1 virus in massive numbers. It hasn’t been confirmed definitively whether the sea lions are spreading the virus to each other or are contracting it from birds or H5N1-infected water.
Here’s the key question: If H5N1 can achieve spread in minks and possibly sea lions, why not humans? We are also mammals. It is true that the farmed minks were confined in close quarters, like chickens on a poultry farm, so that may have contributed. But humans also live in high densities in many cities around the world, providing the virus similar tinder should a human-compatible variant arise.
3. What features could help H5N1 spread well in humans?
Birds experience influenza as a gastrointestinal infection and spread flu predominantly through defecating in water. By contrast, humans experience influenza as a respiratory infection and spread it by breathing and coughing.
Over the centuries, some of these avian influenza viruses have been passed from birds to humans and other mammalian species, although this is a relatively rare event.
This is because bird influenza viruses must mutate in several ways to infect mammals efficiently. The most important mutational changes affect the tissue tropism of the virus – its ability to infect a specific part of the body.
Avian flu viruses have evolved to infect cells of the intestine, while human flu viruses have evolved to infect cells of the respiratory tract. However, sometimes a flu virus can acquire mutations that allow it to infect cells in a different part of the body.
Which cells influenza infects is partially dictated by the specific receptor that it binds. Receptors are the molecules on the surface of host cells that a virus exploits to enter those cells. Once viruses are in cells, they may be able to produce copies of themselves, at which point an infection has been achieved.
Both human and bird influenza viruses use receptors called sialic acids that are common on the surfaces of cells. Bird influenza viruses, such as H5N1, use a version called α2,3-linked sialic acid, while human flu viruses use α2,6-linked sialic acid – the predominant variant in the human upper respiratory tract. Thus, to become efficient at infecting humans, H5N1 would likely need to mutate to use α2,6-linked sialic acid as its receptor.
This is a concern because studies have shown that only one or two mutations in the viral genome are enough to switch receptor binding from α2,3-linked sialic acid to the human α2,6-linked sialic acid. That doesn’t seem like much of a genetic obstacle.
4. Why don’t we make a vaccine just in case?
With avian influenza viruses, it is not possible to make effective human vaccines in advance, because we don’t know exactly what the genetics of the virus will be if it starts to spread well in humans. Remember that the seasonal flu vaccine must be remade every year, even though the general types of flu viruses that it protects against are the same, because the specific genetic variants that affect humans change from year to year.
Right now, the best way people can protect themselves from H5N1 is to avoid contact with infected birds. For more information about prevention, especially for people who keep domesticated birds or are bird-watching hobbyists, the Centers for Disease Control has a list of guidelines for avoiding H5N1 and other bird flu viruses.
Sara Sawyer, Professor of Molecular, Cellular and Developmental Biology, University of Colorado Boulder; Emma Worden-Sapper, PhD Student in Molecular, Cellular and Developmental Biology, University of Colorado Boulder, and Sharon Wu, PhD Student in Interdisciplinary Quantitative Biology and Molecular, Cellular, and Developmental Biology, University of Colorado Boulder
This article is republished from The Conversation under a Creative Commons license.
Read the original article.