By Esther Landhuis, Undark Magazine.
For as long as he can remember, Ken Pressey has had severe allergies to cats. They would trigger hives, runny nose, and watery eyes. Still, like many of the tens of millions of people in the United States who suffer from allergies, Pressey for years did not bother getting treated, or even diagnosed. When cats came near, he just avoided them.
But that tactic has gotten tougher. During the pandemic, Pressey started dating a woman he’s now engaged to marry — and she has two cats. Being with the cats “was absolute chaos,” said the 30-year-old, who lives in Seattle. “I started having asthma attacks.”
Pressey’s primary care physician suggested allergy shots. This century-old approach, a form of immunotherapy, works by exposing the body to small, increasing doses of the culprit substance. Unlike over-the-counter pills and nasal sprays, which only relieve symptoms, shots address the root cause: They help the body build long-term tolerance to the allergens. The treatment is not a cure, but experts say it can bring relief in around 85 percent of patients who try it. And it’s not just a matter of curbing some sneezing. Beyond springtime sniffles, allergies make it hard to concentrate, leading to missed work and school. They can also disrupt sleep, trigger asthma, and contribute to mood disorders.
The procedure for alleviating this misery with allergy shots requires time and diligence. Typically, patients need injections once or twice a week for the first three to six months, then monthly jabs for three to five years. Each office visit also requires a half hour of monitoring after the shot in case of serious reactions, such as wheezing or throat swelling, which are rare but need immediate attention if they occur.
With these scheduling demands, allergy shots were a no-go for Pressey, an engineer with the United States Merchant Marines who often works overseas for months at a time. “I would not be able to keep up,” he said. While looking into alternatives, he recalled a conversation about allergy treatments while stationed in Europe several years earlier, when he heard a coworker say, “We do allergy drops. We don’t do shots. Why would you want to get stabbed by a needle?”
His colleague was referring to a form of sublingual immunotherapy, or SLIT, which builds immune tolerance to allergens administered daily under the tongue. The drops are formulated using the same liquid extracts in skin-based allergy tests, and research suggests the approach works — and is safe for patients to do at home. SLIT drops are a mainstay in Europe, Canada, and Latin America. In the United States, although some medical providers offer the drops off-label, prescribing the treatment remains limited for complex reasons related to regulatory purview and clinic revenue.
That means accessing SLIT drops can be tricky, even for highly motivated patients. “I did quite a bit of extensive reading,” Pressey said. The hardest part, he added, was finding a SLIT provider. Although he managed to connect with several doctors who offer the drops, their clinics were far away. Eventually Pressey went to a forum for allergies on Reddit, which led him to try a consult with Curex, one of more than a half dozen virtual health companies that have started selling allergy tests and SLIT directly to consumers.
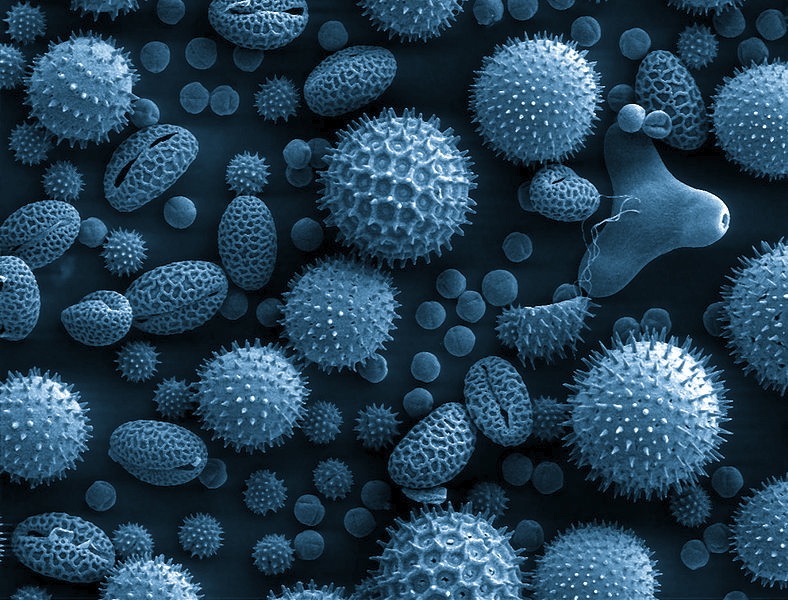
Some of these companies launched during the pandemic when telehealth was rising and Covid concerns kept some allergy sufferers from going to clinic to get shots. The companies’ services focus on diagnosis and treatment of environmental allergies such as pets, dust, pollens, and grasses.
As more health services move online, patients have greater access to treatments but often sacrifice the continuity of traditional physician-patient relationships. As with other areas of medicine, finding allergy care has become a buyer-beware dilemma: Financial incentives and legal complications prevent SLIT from going mainstream with allergists, and so the challenge of making this treatment available and cost-effective has largely landed in the hands of non-allergist practitioners and business executives.
Allergen immunotherapy traces its roots to a pioneering experiment published in 1911. In that study, a pair of young British researchers rounded up patients and showed that injecting their arms with grass pollen toxins could calm their hay fever — which the researchers measured by dripping pollen extract into the patients’ eyes and noting the extent of burning and itching. With little understanding of the cells and molecules involved, physicians refined this method and, in 1954, confirmed its benefits in a double-blind trial.
As the shots regimen gained popularity with physicians, the procedure proved quite safe overall, but news of several patient deaths in the early 1980s led some researchers to explore other ways to treat allergies without injections. Their efforts gave rise to sublingual immunotherapy — the liquid drops now offered by direct-to-consumer companies — and, initially, otolaryngologists, or ear, nose, and throat specialists saw potential in what appeared to be a gentler, more convenient allergy treatment.
Otolaryngology is primarily a surgical specialty. But allergies lie at the root of some of the complications that ENT physicians treat, and often present a roadblock. Whenever allergies cropped up as an underlying cause for his patients’ polyps and nasal disease, they “would never go for allergy therapy because, you know, it was always just shots,” said Chris Thompson, an ENT-trained head and neck surgeon in Austin, Texas, who opened his practice in 1997.
Over the next decade, research continued on sublingual immunotherapy. By 2007, there was “growing consensus that specific sublingual immunotherapy (SLIT) does actually work,” according to one review in the Journal of Allergy and Clinical Immunology. In a 2009 position paper, the World Allergy Organization acknowledged SLIT as a viable treatment. Enterprising doctors began offering this type of immunotherapy.
Still, key details about the technique, such as what doses are needed to achieve benefit, seemed murky. “You could literally go to one doctor and get something that was 10,000 times weaker than what you might get from another doctor,” Thompson said. “There was no standardization.”
Allergists were intrigued by sublingual therapy, but very few at the time offered it in clinic. According to a 2007 survey by the American College of Allergy, Asthma, and Immunology, just 5.9 percent of practicing allergists said they were using SLIT, and by 2011 that figure had only edged up to 11.4 percent. Most respondents cited the lack of FDA-approved products as a barrier.
Nevertheless, interest in sublingual immunotherapy grew in the ENT realm. Professional societies included symposiums about SLIT at their annual meetings and formed subgroups devoted to this new approach. Some otolaryngology group meetings offer courses for physicians to get started with SLIT, Thompson said.
Thompson watched the field a while, noting SLIT’s research progress amid overall trends in allergen immunotherapy, which largely persist today. Shots, despite being the bread and butter of U.S. allergy clinics, are vastly underused. Just 2 or 3 percent of newly diagnosed patients who are recommended for the treatment, actually choose it. Relative to the hordes of patients buying over-the-counter Zyrtec, Thompson said, the number who receive immunotherapy “doesn’t even register.”
One way to make a dent, Thompson figured, was to “offer a therapy people will want.” Thompson opened a second practice, Aspire Allergy & Sinus, in 2012, with a focus on sublingual drops. By then, SLIT seemed promising, Thompson said. “We thought, gosh, this is such a great opportunity.”
A decade later, a similar ambition is fueling direct-to-consumer companies.
There are trade-offs between in-clinic and at-home allergy testing and treatment. When it comes to allergy diagnoses, physicians typically take a detailed clinical history and then use testing, if needed, to confirm the patient’s allergies. Skin testing is the preferred diagnostic among allergists. It has a quick, visual readout — red lumps, or wheals, that form on the patient’s skin 15 to 30 minutes after getting pricked with potential allergens during an office procedure — but it can’t be done at home.
A second type of test checks a patient’s blood for immune proteins called immunoglobulin E (IgE) antibodies. IgE antibodies bind to a specific allergen — say, pollen or peanut — and trigger release of the chemical histamine, which makes people sneeze, itch, swell up, and, occasionally, go into anaphylaxis. Patients can get the blood test at a lab or, increasingly, at home; some online companies sell kits where customers use a provided finger-prick device to apply drops of their blood onto a card, which they can mail to a lab for analysis.
But blood tests can be tricky to interpret, said Robert G. Hamilton, an expert in diagnostic allergy and immunology testing at Johns Hopkins University School of Medicine. A positive result signals the presence of IgE antibody, which “means you’ve become sensitized to the substance,” he said, “but it doesn’t mean you will manifest any allergic symptoms.”
There’s another potential snag. If a patient purchases a home kit and receives results before talking with a physician, confirmation bias can creep in, said Edwin Kim, an allergist-immunologist at the University of North Carolina School of Medicine. If a patient tests positive for dust, for example, the doctor could “ask a thousand questions on dust” until they think they can prove that the patient is “dust-allergic,” he said.
Still, at-home tests and procedures can reach a far broader pool of patients, as it can be difficult to get an in-person appointment with an allergist. At Oregon Health and Science University, “we are booked out through the end of the year,” said allergist-immunologist Shyam Joshi. And at UNC School of Medicine, an academic hub that draws referrals from all over the state and even neighboring states, Kim sees firsthand how patients struggle with their treatment schedule. “We may see them as a great candidate for allergy shots, but you can’t realistically ask people to drive two, three, four hours every week, week after week,” he said.
And allergy shots are not risk-free. While the process goes smoothly for many patients, some develop red, swollen arms after their injection. Occasionally, a shot can trigger an asthma flare-up or a whole-body anaphylactic reaction, said Nikhila Schroeder, an allergist in Huntersville, North Carolina, recalling her own observations about a decade ago when administering shots during her allergy and immunology fellowship. Given all these limitations, “I started to just wonder,” Schroeder said, “Are there any other ways we could do this?”
More recently, that same realization hit Gene Kakaulin, a New York City health care entrepreneur. He was commiserating with a friend in 2018 about his allergies to cats, dust, and pollens, and how things had gotten so bad in his teen years that he tried shots. They were “a pain,” said Kakaulin. “I couldn’t stick with them.”
By contrast, home therapy has lower time demands and less pain and risk — while still desensitizing the immune system by repeated exposures to the allergen. Both approaches produce similar immune changes, though their speed and magnitude, and the types of antibodies involved, can differ. Generally, the immune effects show up faster and stronger with shots, whereas they might take longer with sublingual treatment. It’s hard to compare these changes scientifically — especially since immunotherapy is usually a personalized treatment with dose amounts and escalations tailored to each patient, said Schroeder, whose North Carolina allergy clinic specializes in SLIT.
In studies that have tried to compare the immunotherapy approaches head-to-head, shots seem to do “the same or better” on effectiveness, said Hugh Windom, an allergist in Sarasota, Florida, and on safety, “SLIT always wins.”
Sublingual immunotherapy has been available in the U.S. for decades. SLIT drops, which can treat many different allergens together and are not covered by the Food and Drug Administration, have been offered by at least one allergy clinic since 1970, and by pioneering ENT physicians since the 2010s. In 2014, the FDA approved several tablets that dissolve under the tongue. Three tablets treat grass or ragweed allergies, and a fourth gained approval in 2017 for dust mite allergies.
Still, only about 15 percent of some 2 million allergy immunotherapy patients in the U.S. are using a sublingual version, with the majority on drops, according to market research provided to Undark by Jorge Alderete, who has advised direct-to-consumer allergy companies and other health care startups, and serves on the board of a private equity-backed allergy practice in Houston. An estimated 85 percent of U.S. allergy immunotherapy patients are receiving shots.
One reason is tradition. “We are, of course, wedded to shots because we’ve been doing them for a hundred years,” said Windom.
Another reason relates to versatility. Most allergy patients are allergic to more than one substance, yet allergists tend to prefer FDA-approved products — SLIT tablets — and they only treat a single allergen. Shots, on the other hand, can be tailored to treat many of the patient’s allergens at once. In use for more than a century, allergy shots came to be regulated by the FDA and typically get covered by insurance. SLIT drops can also be customized for multiple allergies, but since the extracts are not FDA-approved for under-the-tongue use and do not have a billing code, patients often must pay out of pocket.
Clinic revenue also plays a role. When an allergist sees a patient and recommends a medication, such as an antihistamine, they charge for a single office visit. Allergy shots bring in more revenue. (Exactly how much revenue can be difficult to estimate, as costs can vary significantly clinic to clinic.) When a patient goes on the shots, three to five years of office treatments at weekly to monthly intervals can amount to dozens of billable visits. Plus, with each visit the clinic charges for mixing the specialized treatment and administering the shot, said Alderete. From a business perspective, he said, immunotherapy is “an annuity.”
Unlike shots, which are billed as a procedure, SLIT tablets are a prescribed drug. “If you’re going to ask an allergist, hey, do you want to do shots and make money off of it, or prescribe something to Walgreens,” Kim said, it’s understandable that tablets aren’t preferred by allergists in the U.S. Customized SLIT drops are prepared in-house at some clinics, or physicians can send the prescription to a compounding pharmacy.
In the drops form, SLIT does square well with shots on versatility — both can address combinations of allergens with adjustable dosing and escalations — but per-patient profit margins can be higher with shots, said Alderete.
This is in part because of doctors’ costs associated with purchasing and preparing the allergen extracts. Though different forms of immunotherapies use the same source material, SLIT preparations can be “significantly more concentrated than even the top doses of allergy shots,” said allergist and immunologist Sakina Bajowala, who offers both treatments at her allergy practice outside of Chicago. In one analysis of immunotherapy regimens for birch allergy, the total amount of allergen administered over the course of a year was 30 times greater with SLIT compared with shots. And office-made SLIT, Bajowala said, can make doctors’ margins even slimmer: “The more extract used, the more costly the drops.”
ENT practices are more willing to offer a less lucrative therapy because, unlike allergists, their revenue mostly comes from surgeries, so SLIT is “a bit of an ancillary service,” said Thompson.
But on the whole, SLIT drops remain far from mainstream, even as interest in this mode of treatment grows.
After hearing about his friend’s needle-free therapy — SLIT drops — Kakaulin made a round of calls to practices in New York so he could try SLIT himself. His symptoms improved “within a few months,” which helped him sleep and exercise better, he said. To this day, the drops remain a part of Kakaulin’s morning routine — “two minutes under the tongue right after brushing teeth when I shave.”
Along the way, he co-founded Curex, one of several online allergy companies that got off the ground during the pandemic as telemedicine soared. While just 1 percent of allergy appointments took place virtually before the pandemic, that figure jumped to 54 percent one month into lockdown. Across medicine, telehealth shot up 78-fold between February 2020 and April 2020, according to an analysis, from the consulting firm McKinsey, and after a year remained 38 times higher than pre-pandemic.
Meanwhile, brick-and-mortar clinics took a hit. “A lot of allergy offices closed because of Covid concerns, and then people who were supposed to get shots were left out in the cold,” said Kim.
Direct-to-consumer allergy companies capitalized on this perfect storm, luring customers with glowing testimonials, free quizzes, and heaps of online advertising. Their social media ads showcase sublingual drops as a “convenient alternative to allergy shots” with “no trips to the doctor’s office or prickly needles.”
Some of these companies also offer allergy testing. Curex can send a phlebotomist to administer blood tests to patients with eligible zip codes. Wyndly, a company headquartered in Lakewood, Colorado, ships a $249 test kit to the customer’s home. New York City-based Nectar also sells home tests and lets patients upload results of previous allergy testing. Based on test results and a medical consult, the companies sell formulated sublingual drops on subscription plans, some at $99 per month or less. “We think there are tens of millions of Americans who could benefit,” said Kakaulin, who had helped start a prescription savings company before launching Curex in 2020.
To reach those millions of potential customers, companies that sell allergy drops face similar financial challenges as allergy practices. The average SLIT patient “produces 70 or 80 percent less revenue than an allergy shot patient,” Kakaulin said. So instead of trying to maximize per-patient profit, Curex is trying to “maximize some of our efficiencies and provide everyday low prices,” he said.
Toward this end, nationwide direct-to-consumer companies, as well as large multi-site allergy practices, can negotiate lower pricing on allergen extracts and other supplies because they order huge volumes. Small practices often do not get these discounts and thus have higher backend costs if they choose to offer off-label SLIT.
Amid these financial considerations, there’s also a mindset difference between serving patients and winning customers. With a business model that relies on “one thing,” Bajowala said, it’s in a direct-to-consumer company’s interest to create ads that say, “well, the thing we’re offering is the best, so why would you even want to consider the other thing?”
Some allergists worry that direct-to-consumer companies hasten a broader trend: the decline of the practitioner-patient relationship. When patients begin a new treatment, they “need to know when is it going to start working, how to monitor for side effects, and if there’s a problem, who are you going to go to?” said Anne Maitland, an allergist-immunologist at Icahn School of Medicine at Mount Sinai in New York City and the director of allergy and immunology at the Metrodora Institute in Salt Lake City, Utah.
| Support Undark Magazine Undark is a non-profit, editorially independent magazine covering the complicated and often fractious intersection of science and society. If you would like to help support our journalism, please consider making a donation. All proceeds go directly to Undark’s editorial fund. Give Now |
At direct-to-consumer companies, details about what’s in the treatment and who’s providing the medical care are also somewhat of a black box. Pressey, the Merchant Marine with the cat allergy, said that if he were to request a consult at Curex, for instance, it would not be with the provider who did his intake. “That person doesn’t work there anymore,” he said. And if he ever wanted to stop his subscription and continue SLIT treatment elsewhere, Curex does not “give you the exact mixture that you’re getting treated for,” Pressey said.
As for staffing, Nectar relies heavily on primary care physicians with training in allergy immunotherapy, but a public relations spokesperson denied a request to interview one of these providers. Regarding the number of doctors in the Curex network, Kakaulin declined to answer. “I’d rather not talk about specifics of the business,” he said. “We’d prefer to have certain information kind of private.”
While the approach lacks transparency, patients often can’t access information in traditional health care settings, either. In a health care system that favors standardized protocols, insurance reimbursements and clinic business priorities may compel physicians to recommend certain treatments, making it hard for patients to learn about the full spectrum of options, said Schroeder, whose clinic offers SLIT using a direct-care model, where patients pay the provider directly rather than using traditional fee-for-service insurance.
In fact, the allergy clinic might be one of the hardest places to get clear information about treatment options. That’s in part because of a lawsuit from almost a decade ago. In 2014, the American Academy of Allergy, Asthma & Immunology (AAAAI), American College of Allergy, Asthma & Immunology (ACAAI), and several other allergy groups were sued by United Allergy Services, a company that helps primary care physicians and other non-specialists diagnose and treat allergies.
The company alleged that allergists who decried UAS practices were restricting the market and limiting patient access to allergen immunotherapy. As part of a settlement, the allergy groups issued a policy statement requiring members to minimize litigation risk by complying with antitrust laws. As Matt Bell, an allergist in Fayetteville, Arkansas, explained it, the lawsuit is “why we are hesitant to talk.” The settlement terms “basically stated that AAAAI had to keep their mouths shut,” said David Stukus, an allergist at Nationwide Children’s Hospital in Columbus, Ohio, who declined to speak about specific companies or services.
And depending on where and how a patient finds SLIT, their experiences can vary widely. With rising demand for allergy care and limited allergist availability, patients can get allergy treatment from many sources besides their local allergist — including ENT practices, primary care doctors, pediatricians, urgent care, emergency rooms, naturopathic doctors, and direct-to-consumer companies. “If you do SLIT at different places, it won’t necessarily be the same. The people may have different levels of expertise,” said Schroeder, who learned the ins and outs of sublingual therapy at Allergy Associates of La Crosse, a Wisconsin clinic that has offered this treatment for environmental and food allergies since 1970. Nevertheless, she said, there’s a role for all these various avenues as long as patients understand the complexities and “know what they’re pursuing.”
So far, the direct-to-consumer drops seem to be working well for Pressey. Before starting treatment in 2021, he struggled with frequent allergy-induced asthma attacks. “I couldn’t make it 24 hours with a cat in the house,” he said in a recent interview. Now “it’s about two and half weeks before I even remember that I have asthma.”
Pressey still has questions about the therapy and about Curex — like how long the benefits will last and whether the company will survive. Even when scouring Reddit in spring 2021, he could not find answers to these questions. Nevertheless, “I’m a firm believer in new technology,” he said. “You know what, if no one tries it, then no one will ever get the answers.”
This article was originally published on Undark.
Read the original article.



