
Michael Noetel, The University of Queensland
At least one in ten people have depression at some point in their lives, with some estimates closer to one in four. It’s one of the worst things for someone’s wellbeing – worse than debt, divorce or diabetes.
One in seven Australians take antidepressants. Psychologists are in high demand. Still, only half of people with depression in high-income countries get treatment.
Our new research shows that exercise should be considered alongside therapy and antidepressants. It can be just as impactful in treating depression as therapy, but it matters what type of exercise you do and how you do it.
Walk, run, lift, or dance away depression
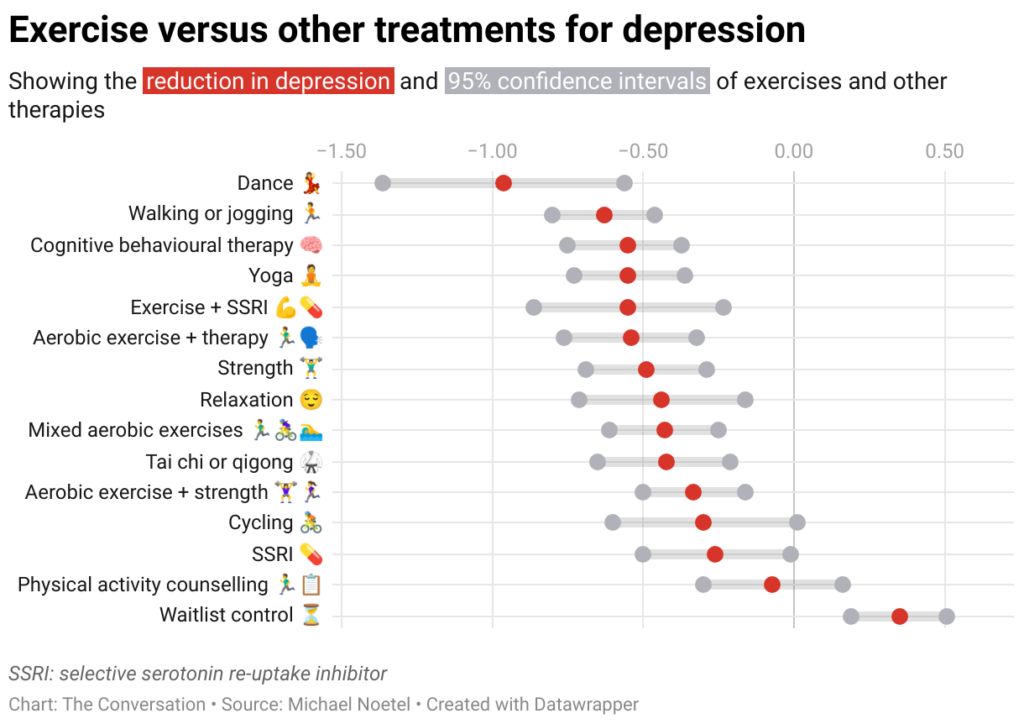
We found 218 randomised trials on exercise for depression, with 14,170 participants. We analysed them using a method called a network meta-analysis. This allowed us to see how different types of exercise compared, instead of lumping all types together.
We found walking, running, strength training, yoga and mixed aerobic exercise were about as effective as cognitive behaviour therapy – one of the gold-standard treatments for depression. The effects of dancing were also powerful. However, this came from analysing just five studies, mostly involving young women. Other exercise types had more evidence to back them.
Walking, running, strength training, yoga and mixed aerobic exercise seemed more effective than antidepressant medication alone, and were about as effective as exercise alongside antidepressants.
But of these exercises, people were most likely to stick with strength training and yoga.
Antidepressants certainly help some people. And of course, anyone getting treatment for depression should talk to their doctor before changing what they are doing.
Still, our evidence shows that if you have depression, you should get a psychologist and an exercise plan, whether or not you’re taking antidepressants.
Join a program and go hard (with support)
Before we analysed the data, we thought people with depression might need to “ease into it” with generic advice, such as “some physical activity is better than doing none.”
But we found it was far better to have a clear program that aimed to push you, at least a little. Programs with clear structure worked better, compared with those that gave people lots of freedom. Exercising by yourself might also make it hard to set the bar at the right level, given low self-esteem is a symptom of depression.
We also found it didn’t matter how much people exercised, in terms of sessions or minutes a week. It also didn’t really matter how long the exercise program lasted. What mattered was the intensity of the exercise: the higher the intensity, the better the results.
Yes, it’s hard to keep motivated
We should exercise caution in interpreting the findings. Unlike drug trials, participants in exercise trials know which “treatment” they’ve been randomised to receive, so this may skew the results.
Many people with depression have physical, psychological or social barriers to participating in formal exercise programs. And getting support to exercise isn’t free.
We also still don’t know the best way to stay motivated to exercise, which can be even harder if you have depression.
Our study tried to find out whether things like setting exercise goals helped, but we couldn’t get a clear result.
Other reviews found it’s important to have a clear action plan (for example, putting exercise in your calendar) and to track your progress (for example, using an app or smartwatch). But predicting which of these interventions work is notoriously difficult.
A 2021 mega-study of more than 60,000 gym-goers found experts struggled to predict which strategies might get people into the gym more often. Even making workouts fun didn’t seem to motivate people. However, listening to audiobooks while exercising helped a lot, which no experts predicted.
Still, we can be confident that people benefit from personalised support and accountability. The support helps overcome the hurdles they’re sure to hit. The accountability keeps people going even when their brains are telling them to avoid it.
So, when starting out, it seems wise to avoid going it alone. Instead:
- join a fitness group or yoga studio
- get a trainer or an exercise physiologist
- ask a friend or family member to go for a walk with you.
Taking a few steps towards getting that support makes it more likely you’ll keep exercising.
Let’s make this official
Some countries see exercise as a backup plan for treating depression. For example, the American Psychological Association only conditionally recommends exercise as a “complementary and alternative treatment” when “psychotherapy or pharmacotherapy is either ineffective or unacceptable”.
Based on our research, this recommendation is withholding a potent treatment from many people who need it.
In contrast, The Royal Australian and New Zealand College of Psychiatrists recommends vigorous aerobic activity at least two to three times a week for all people with depression.
Given how common depression is, and the number failing to receive care, other countries should follow suit and recommend exercise alongside front-line treatments for depression.
I would like to acknowledge my colleagues Taren Sanders, Chris Lonsdale and the rest of the coauthors of the paper on which this article is based.
If this article has raised issues for you, or if you’re concerned about someone you know, call Lifeline on 13 11 14.
Michael Noetel, Senior Lecturer in Psychology, The University of Queensland
This article is republished from The Conversation under a Creative Commons license.
Read the original article.


