From the National Cancer Institute by Sharon Reynolds
The human gut contains trillions of bacteria. Some play helpful roles, like helping to digest food. Others can be problematic, causing conditions like stomach ulcers.
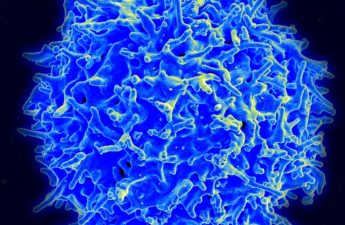
Tumors that arise in the lower intestines, which includes the colon and rectum, are constantly exposed to a wide range of gut bacteria. This intimate physical relationship has led researchers to wonder if some species of bacteria could be affecting the growth of colorectal tumors.
Over the last decade, one such species, called Fusobacterium nucleatum, has been strongly implicated as a potential contributor to colorectal cancer growth. Although F. nucleatum is normally found in the mouth, studies have also found increased numbers of it in the intestines of people with colorectal tumors compared with people without cancer.
In a new study, published on March 20 in Nature, NCI-funded researchers have pinpointed a single type of F. nucleatum that appears to be the cancer-fueling culprit scientists have been searching for.
In studies in the lab, they showed that this type of F. nucleatum could survive for an extended time in conditions that mimicked the stomach’s acidic environment. And in mice, its presence increased the number of precancerous growths called adenomas in the large intestine. It also produced compounds that can create a beneficial environment for tumor growth.
In tissue samples taken from people with colorectal cancer, this type of F. nucleatum was the only type more likely to be found in tumor tissue than in nearby healthy tissue. And people with colorectal cancer were five times as likely to have this bacterium in their stool than people without the disease.
“It sounds scary, but this is good information to have,” said Susan Bullman, Ph.D., of Fred Hutch Cancer Center, who co-led the study. “Microbes are manipulatable—you can target them. So [as] we see that this microbe is getting to tumors and may be contributing actively to disease progression, we can harness that information and think about how to prevent that.”
The findings highlight the need for a more comprehensive understanding of the behavior of different microbes in the lower intestines, added Phil Daschner, a program director with NCI’s Division of Cancer Biology who was not involved with the study.
“The microbes in our gut include bacteria, but also fungi and viruses,” Daschner said. “And [some] may be helping to promote tumor growth.”
From the mouth to the gut
Even in its natural home, the mouth, F. nucleatum is not our friend. “In the oral cavity, it’s considered a ‘bridging’ organism,” explained Christopher Johnston, Ph.D., the study’s other co-leader, also from Fred Hutch. That means it helps bind together other microorganisms in the mouth to produce the sticky, cavity-causing substance called dental plaque, which in turn can help cause gum disease.
Previous studies have found F. nucleatum in and around colorectal tumors—not just those located in the colon and rectum, but also in colorectal cancer that has metastasized elsewhere in the body.
“But not all [types of] F. nucleatum are the same,” Dr. Bullman explained. “There’s high variation within these organisms and in what they’re capable of doing.”
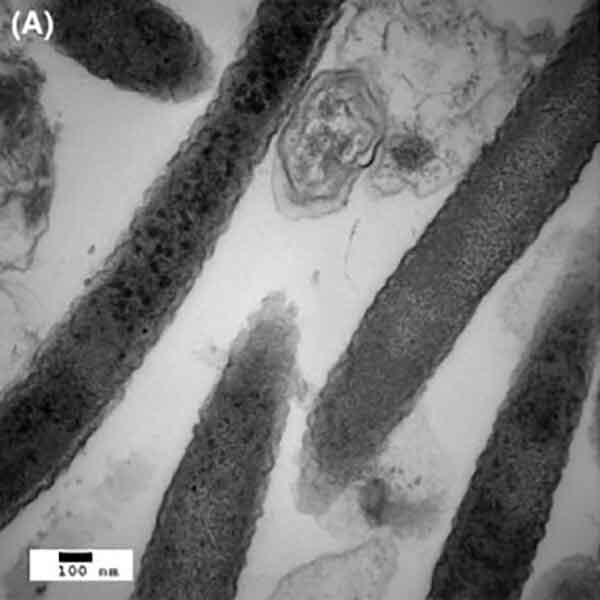
To get a more specific picture of which types of F. nucleatum may be attracted to colorectal tumors, the researchers first analyzed the genomes of F. nucleatum types taken from human colorectal tumors and from the mouths of people without cancer. Out of its several known subspecies, only one, called F. nucleatum animalis (or Fna), was routinely found in the tumor samples.
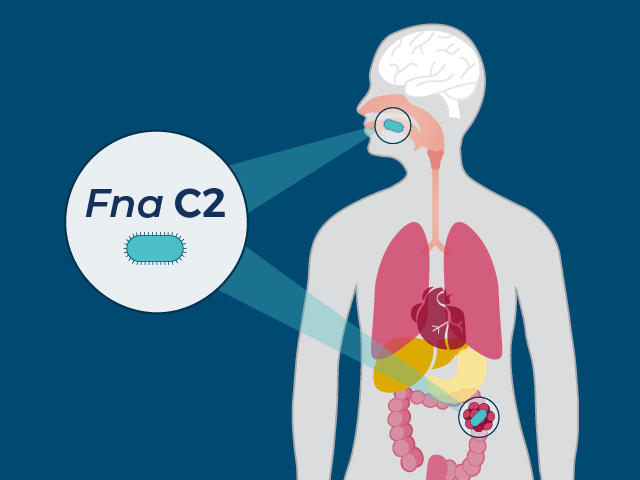
Additional genetic analyses revealed that Fna could be divided even further, into two separate groups. While both groups were found in about equal proportions in the mouth, only one, dubbed Fna C2, was found in colorectal tumor samples in substantial numbers.
As expected, the two groups were genetically very similar. However, by sequencing their complete genomes, the team was able to tease out several genetic differences among them that could explain Fna C2’s ability to set up shop in tumors.
Those differences included Fna C2’s higher resistance to acid, which could allow it to potentially reach the intestines directly from the mouth, through the stomach. Fna C2 also had the ability to hide inside certain tumor cells, which could protect it from the immune system. And it was able to use nutrients found in the gastrointestinal tract, which are very different from those found in the mouth.
“These are unique features that allow [Fna C2] to survive this transit and to set up house in the lower gastrointestinal tract,” said Dr. Bullman.
Does Fna C2 help start as well as fuel tumors?
The team next conducted experiments in mice to try to get a better handle on Fna C2’s ability to help tumors form and grow.
That work showed that Fna C2 could slightly increase the formation of adenomas in the colon. It also produced changes in energy availability for cancer cells in the intestines that could create an environment favorable to tumor formation.
Bactria May Aid Growth of Colorectal Cancer
Study links specific bacterial species to growth, spread of this common cancer.
To date, no mouse model has been able to closely mimic bacterial behavior in the human colon, Dr. Bullman explained. For example, some of the human proteins that the bacteria binds to or uses to grow aren’t found in mice.
This has made studying the contribution of bacteria to the early formation of tumors difficult, she added. “So while we think this microbe is important in cancer progression, for its role in cancer initiation, the jury’s still out,” she said.
Going back to humans, the team looked for the two Fna groups in tissue samples taken from more than 300 people with colorectal cancer. Only Fna C2 was found in greater numbers in tumor tissue than in samples taken from adjacent normal tissue.
The researchers also measured Fusobacterium types found in stool samples from people with colorectal cancer and people without the disease. Whereas almost 30% of people with colorectal cancer had Fna in their stool, less than 5% of people in the healthy comparison group did.
Targeting a problematic bacterium
“What’s probably the most important [thing] about this research is the potential to identify [new] treatments,” Daschner said. “If you can inhibit Fna C2, you might be able to either prevent polyps from progressing to cancer or prevent already-formed tumors from getting worse.”
Previous research in mice showed that using antibiotics to knock out Fusobacterium could slow the growth of colorectal cancer. But antibiotics can kill other bacteria as well, which could lead to unexpected effects on a tumor or on beneficial bacteria in the rest of the body, said Dr. Bulllman.
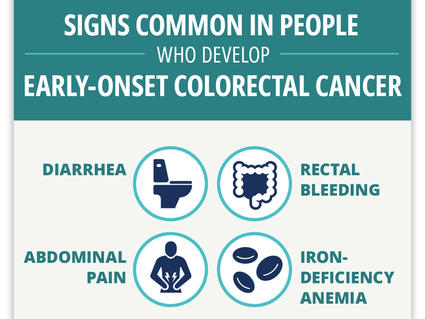
Can Colorectal Cancer in Younger Adults Be Found Early?
Researchers find four “red flag” signs that may identify colorectal cancer early in younger adults.
“But identifying this specific [type] may allow us to identify [drugs] that can specifically target this subgroup, because it’s genetically distinct,” she said.
Dr. Johnston’s team hopes to eventually use Fna C2 to create what they call microbial cellular therapies, using the bacterium like a Trojan horse to deliver cancer drugs into a tumor.
“Because this [bacterium] has such an intimate relationship with cancer, if we can strip out the parts that make it [dangerous] but keep the parts that allow it to travel to and colonize tumors, that could be a new strategy for delivering drugs directly into these tumors,” he explained.
The discovery of this type of F. nucleatum may eventually have implications for colorectal cancer screening, said Daschner.
The presence of Fna C2 alone in stool wouldn’t be enough to diagnose cancer or polyps, he explained. But future studies could look at whether adding it to existing tests that look for blood or cancer DNA in the stool may potentially help identify more people who need a follow-up colonoscopy, he added.
The relationships between microbes that can cause gum problems and the risk of diseases elsewhere in the body are still under study. “But maintain your oral health,” said Dr. Johnson.
Previous research has found that people with gum disease had an increased risk of several different cancer types, he explained. “So a link between oral health and cancer is certainly there.”
“The mouth is such a unique environment; [and] it’s the gateway into the body for most pathogens,” Dr. Johnson added. “It makes sense to keep it protected.”
Subscribe to the NCI’s “Cancer Currents” blog