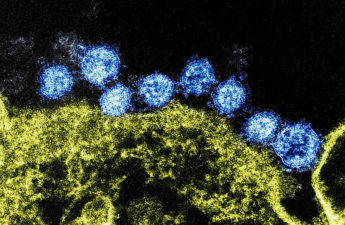
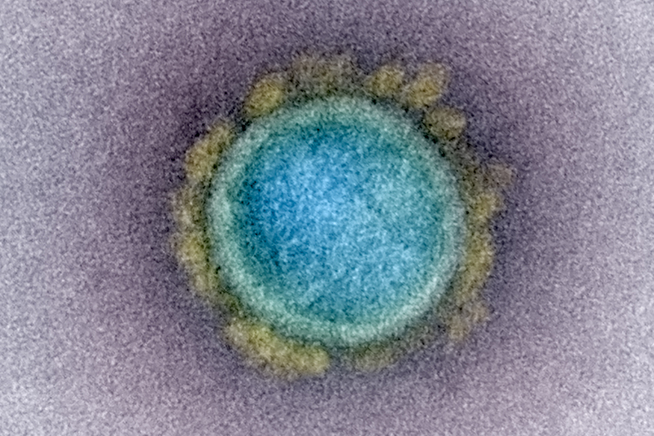
COVID summer continues to heat up
The summer’s COVID-19 wave is continuing, with the latest wastewater surveillance data detecting “high” virus activity levels across the majority of the U.S. and “very high” levels in 19 states, per Centers for Disease Control and Prevention data. . . . Hospitalizations remain low. However, the virus still poses a risk to the elderly and immunocompromised.Axios.
Gen X and millennials at higher cancer risk than older generations
Cancer rates for 17 of the 34 most common cancers are increasing in progressively younger generations, a large new study shows.
. . . Cancers with the most significant increased risk are kidney, pancreatic and small intestine, which are two to three times as high for millennial men and women as baby boomers. Millennial women also are at higher risk of liver and bile duct cancers compared with baby boomers. WashingtonPost.
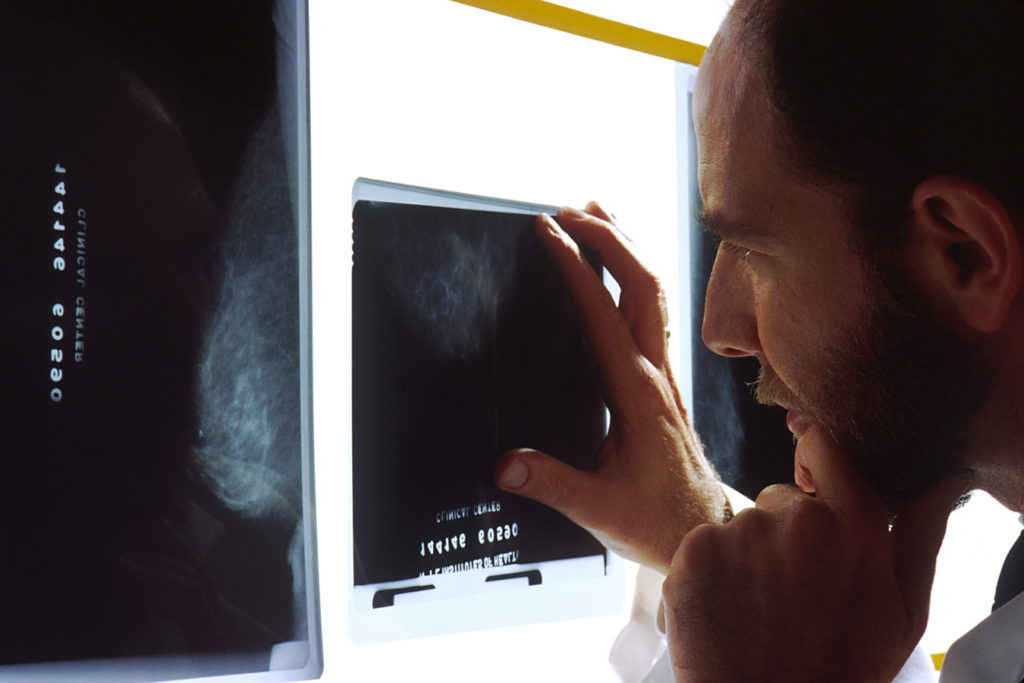
Double Mastectomy Shows No Survival Benefit For Most Breast Cancer Patients, Study Says
A new study published in JAMA Oncology followed more than 650,000 women with breast cancer in one breast for up to 20 years and found that women who underwent double mastectomy were less likely to develop cancer in the other breast, but didn’t live any longer, on average, than women who didn’t undergo double mastectomy. In other words, women who had a lumpectomy or a mastectomy on the affected side but kept their other breast did just as well from a survival benefit as women who had both breasts removed. They say this may not apply to women with the BRCA1 or BRCA2 genes which puts them at much higher risk of breast cancer. CBSNews.
Bird Flu Cases Are Going Undetected, New Study Suggests. It’s a Problem for All of Us.
. . . As bird flu cases go underreported, health officials risk being slow to notice if the virus were to become more contagious. A large surge of infections outside of farmworker communities would trigger the government’s flu surveillance system, but by then it might be too late to contain. KFFHealthNews.

What’s behind new combined urgent care-ER facilities
One-stop ER-urgent care shop includes both but at very different prices
. . . At the facilities, doctors decide whether a patient needs urgent or emergency care — the health system bills accordingly — and inform the patient of their decision before testing or treatment begins. Emergency care is almost always more expensive than urgent care. For patients who might otherwise show up at the ER with an urgent care-level problem — a small cut that requires stitches or an infection treatable with antibiotics — the savings could be hundreds or thousands of dollars. . . . While no research has been conducted on this new hybrid model, consumer advocates worry that hospitals are more likely to route patients to costlier ER-level care whenever possible. WashingtonPost.
Nearly Half Of Insured Americans Get Surprise Expenses In Medical Bills, Survey Finds.
Nearly half of Americans with health insurance said they received a recent medical bill or a charge that “should have been free or covered by their insurance,” according to a survey released Thursday. The survey, from the Commonwealth Fund in New York City, found 45% of working-age consumers last year were erroneously billed, however, fewer than half of those patients challenged their health insurance company or a medical provider about the unexpected charges. USAToday.
Most U.S. Adults Don’t Know They Can Fight Insurance Denials, New Study Finds
Despite laws in states like Pennsylvania, New Jersey and Delaware that aim to ensure people have access to affordable health care services, research shows that patients still receive unexpected medical bills and face insurance denials — and few of them choose to take action. A new national survey report released Thursday by the Commonwealth Fund shows that fewer than half of people who experienced insurance denials and billing issues actually fought the decisions. WHYY
After Private Equity Takes Over Hospitals, They Are Less Able To Care For Patients, Say Top Medical Researchers
After private-equity firms acquire hospitals, the facilities’ assets and resources diminish significantly, leaving the facilities less equipped to care for patients, according to a new study . . . Published Tuesday in the Journal of the American Medical Association, the research highlights a pattern of asset stripping at health care facilities purchased by private-equity firms, its researchers said, and is the first study to analyze the activity nationwide. . . . The study found that during the two years after a private-equity acquisition, total capital assets at private equity-acquired hospitals declined by 15% on average while assets rose by an average of 9% at other hospitals. That makes for a net difference of 24%, the researchers found, equivalent to a loss of $28 million in total assets per hospital. NBC.
Trust in Doctors Crashed During the COVID Pandemic — And Remains Low
Putting financial motives over patient care was top reason for patient mistrust, survey found
Trust in physicians and hospitals decreased sharply during the COVID-19 pandemic, and higher levels of trust were tied to greater odds of getting vaccinated for COVID-19 or influenza, according to a survey study of U.S. adults . . . the proportion of adults who agreed they had “a lot of trust” in physicians and hospitals declined from 71.5% in April 2020 to 40.1% in January 2024 . . . Participants with the two lowest levels of trust identified the following reasons: financial motives over patient care (35%), poor quality of care and negligence (27.5%), influence of external entities and agendas (13.5%), and discrimination and bias (4.5%).MedPageToday.
Weight loss drugs like Wegovy may trigger eating disorders in some patients, doctors warn
Abuse of weight loss drugs is nothing new, but “nothing compares to the phenomenon that we’re seeing right now with these GLP-1s,” one provider said.
. . . In some cases, a person’s brain may interpret such dramatic, sudden weight loss as starvation, Hildebrandt said, making people more obsessive about food. People who are taking these new weight loss drugs, he posited, may then find themselves compelled to further limit how much food they eat, even when it endangers their health. NBC.
Experiencing Racism May Physically Change Your Brain
Scientists know that Black people are at a greater risk for health problems like heart disease, diabetes and Alzheimer’s disease than white people. A growing body of research shows that racism in health care and in daily life contributes to these long-standing health disparities for Black communities. Now, some researchers are asking whether part of the explanation involves how racism, across individual interactions and systems, may physically alter the brain. NPR.

As wildfires rage, what is the smoke doing to our health and bodies?
Scientists are discovering just how toxic wildfire smoke is to the body – here’s what to know and how to stay safe
. . . Researchers are still trying to understand exactly why, but wildfire smoke contains a toxic brew of compounds – including volatile organic compounds, aromatic hydrocarbons and heavy metals. That’s partly due to what is burning: when buildings go up in flames, the smoke will include metals, cleaners and many different types of substances – some that are carcinogenic – that become aerosolized. “All of these things make it worse for our bodies than the fossil fuel pollution that we’re always breathing,” [says Dr Lisa Patel, a pediatrician and executive director at the Medical Society Consortium on Climate and Health.] TheGuardian.
Expert Panel: Target These 14 Factors to Cut Dementia Incidence by Nearly Half
Prevention approaches should aim to decrease risk factor levels early (ie, the earlier, the better) and keep them low throughout life (ie, the longer, the better). Although addressing risk factors at an early stage of life is desirable, there is also benefit from tackling risk throughout life; it is never too early or too late to reduce dementia risk. . . . The potential for prevention is high and, overall, nearly half of dementias could theoretically be prevented by eliminating these 14 risk factors. . .
- Lack of education
- Hearing loss
- Depression
- Head trauma from sports and bike riding
- Physical activity
- Smoking
- Hypertension
- Obesity
- Type 2 diabetes
- Alcohol drinking
- Social isolation
- Air pollution
- Vision loss
- High LDL The Lancet.
Headed to an outdoor concert or event? How to stay safe in the heat.
One key risk you can try to control at outdoor events: dehydration.
. . . Concertgoers and festival attendees expose themselves to multiple heat-related risks, which could lead to issues as minor as heat cramps to more severe situations like heat stroke, which can be fatal. . . . It’s important for everyone to hydrate during extreme temperatures — especially with increased activity and prolonged exposure. “People should be excited about the event but also have a plan to keep hydrated and identify locations to get out of the sun if they are feeling too hot. WashingtonPost.

Long Covid health issues persist in those hospitalised early in pandemic, study finds
Substantial proportion have cognitive and mental health problems years after infection, with some symptoms worsening
. . . While the researchers had no information on the participants’ thinking skills before they got Covid, cognitive tests two to three years later showed that on average patients’ IQs were 10 points lower than expected for their age, education and other factors. One in nine showed signs of “severe cognitive deficits”, which equate to an IQ 30 points lower than expected. TheGuardian.
Risk Of Heart Attack, Stroke Drops After COVID Vaccination, Data Show
A study today involving 46 million adults in England shows that the incidence of both heart attacks and strokes dropped following COVID-19 vaccination compared to the incidence before or without vaccination. The study authors said the incidence of common cardiovascular diseases dropped after every COVID-19 vaccination, but COVID-19 vaccination was associated with slightly increased rates of myocarditis and pericarditis following mRNA-based vaccines, and vaccine-induced thrombotic thrombocytopenia following adenovirus-based vaccines such as the AstraZeneca vaccine. CIDRAP.
Can a 6-second kiss each day lead to a more intimate relationship?
A daily intimacy exercise pioneered by couples therapists and clinical psychologists John and Julie Gottman, the six-second kiss is what it sounds like — taking a few moments out of each day to connect physically with your partner. . . . After studying more than 3,000 couples over 30 years, the Gottmans found that six seconds of intentional intimacy is enough to trigger the release of oxytocin. It’s the same hormone that’s widely believed to be responsible for bonding a baby with its mother; the Gottmans say it builds trust in a relationship by calming down the fear center of the brain. AP.