It’s easier than ever to get prescription drugs online. Should regulators be paying more attention?
BY TERESA CARR
Undark Magazine
IT STARTED WITH A GOOGLE SEARCH for prescription medications I might get online.
Almost immediately, ads from telehealth companies began chasing me around the internet, promising access to drugs to make me prettier, skinnier, happier, and hornier. Several of these companies sell anti-aging creams. While decidedly pro-aging, I don’t love the visible effects of my sun-soaked youth. “Sure,” I thought. “Why not?”
Within the hour I had joined the millions of Americans who get prescription drugs from providers in cyberspace.
MATTERS OF FACT: Exploring the intersection of science & society.
Telehealth, an umbrella term for health care delivered by phone, video chat, or messaging, exploded during the pandemic. Since then, it has become a mainstay of many medical practices. Also riding the telehealth wave is a raft of internet-based companies that facilitate prescribing — and often sell — medications for complaints that because of time, money, or embarrassment people don’t want to discuss with a doctor face-to-face.
Related: When Doctors Are Also Pharmacists
My experience represents the sunny side of direct-to-consumer telehealth. It took about 15 minutes to fill out a medical history, upload photos of my face, and enter my credit card information on forhers.com, a website run by the telehealth company Hims & Hers Health, Inc. Twenty minutes later, a nurse practitioner had prescribed a Hers product containing tretinoin, a well-studied Vitamin A derivative that smooths fine wrinkles and fades dark spots. Six days after that, it showed up at my door.
Compared to the conventional health care system, the process of obtaining the prescription felt like scoring a fast pass at Disneyland.
But last year, urologist Justin Dubin discovered a darker side of DTC telehealth. Alarmed at seeing patients who had been prescribed the hormone testosterone without good medical reason or warnings about side effects, Dubin went undercover as a secret shopper at seven platforms targeting men’s health. Following a script, he described himself as a happily married 34-year-old man bothered by low energy, decreased sex drive, and erectile dysfunction. “I read about low testosterone and its symptoms online,” he told potential prescribers, “and I am worried that I might have it.”
Dubin, who like his alter ego was 34, submitted his own lab results showing healthy hormone levels. “It was pretty clear that I did not need testosterone,” said Dubin, who treats patients at Memorial Healthcare System in Florida. Nonetheless, as he detailed in a study published in JAMA Internal Medicine in December 2022, providers working for six of the seven companies defied medical society guidelines to offer to prescribe him injectable testosterone. They also offered to sell him several other testosterone-boosting drugs and supplements that were inappropriate for his hypothetical case.
“It just seemed like it was just a terrible practice of medicine.”
“This was just egregious, what Dubin found,” said Steven Woloshin, a professor of medicine at Dartmouth. Even though Dubin’s script made it clear that he and his wife wanted to have a child in the near future, half of the telehealth providers offering testosterone failed to warn him that, in addition to other risks, taking the hormone can reduce fertility. “For this simulated patient it could interfere with his goal to have children, and they were treating something he didn’t have,” said Woloshin. “It just seemed like it was just a terrible practice of medicine.”
Woloshin said the paper has big implications about the poor quality of online care: “There’s no reason to think that this is unique to urology.”
In an accompanying editorial, Woloshin, and my former colleague Lisa Gill, an investigative reporter at Consumer Reports, called for better oversight of standalone DTC telehealth services. “Consumers need to be aware of the potential for bad care,” they wrote, “and regulators need to do more to protect them.”
FOR TELEHEALTH, EVERYTHING CHANGED with the onset of the Covid-19 pandemic. In the U.S., telehealth use skyrocketed with lockdowns in the spring of 2020 and then stabilized at 38 times higher than pre-pandemic levels by early 2021, according to a report from the consulting firm McKinsey & Company.
By and large, DTC companies fall into two main business models. Companies such as Teladoc, Amwell, DoctorOnDemand, and MDLivemost closely resemble traditional medical practices. They take insurance, send prescriptions to your pharmacy, and offer a range of services, including urgent care, primary care, psychiatry, mental health counseling, and dermatology.

Last year, urologist Justin Dubin investigated seven DTC platforms targeting men’s health. He found that providers working for six of those companies defied medical society guidelines to offer to prescribe him injectable testosterone. Other experts described his findings as “egregious.” Image: Courtesy of Justin Dubin
Then there are a host of platforms that treat a narrower set of conditions, such as Ro — which focuses on skin, hair, fertility, weight loss, and sexual health — and the men’s health clinics that Justin Dubin shopped. These companies typically don’t take insurance and charge little or nothing for patient visits. Instead, they make money by selling products that their providers prescribe. “It’s simply a route to market for a drug,” said Mark VanderWerf, a telehealth entrepreneur and consultant.
From the patient perspective, the DTC approach has demonstrated benefits, said Ateev Mehrotra, a physician and health care policy scholar at Harvard Medical School who started researching telehealth a decade ago. As I discovered, it’s efficient. No travel time; no scrolling on my phone in a waiting room. “Patients’ time is valuable,” he said. “And the convenience of it is obviously really critical.”
Plus, because of the efficiencies built into the telehealth model, said Mehrotra, “many of these companies can provide care at lower cost.” That’s a huge plus for people facing poor insurance coverage or high deductibles.
Those virtual clinics can also specialize in serving populations that otherwise struggle to get care, said Crystal Beal, a family medicine physician who provides treatment and education through the website QueerDoc. Because many doctors don’t feel confident and comfortable providing gender-affirming care, Beal told me, some of their patients previously had to travel more than 200 miles for appointments. DTC options, they said, are sometimes “really the only option for trans and gender-diverse patients.”
The explosion of DTC telehealth is a direct result of the failures of our health care system, said Ashley Winter, who until recently served as the chief medical officer of Odela, a DTC telehealth company focused on women’s sexual health. Winter previously treated both men and women as a urologist and sexual medicine physician at a large managed care organization, and she said she joined Odela to help more patients: “I was drowning in need.”
WHILE DTC PLATFORMS CAN compensate for some of the shortfalls of America’s health care system, they can also bring out its worst money-grubbing tendencies.
Mehrotra is most concerned about what he refers to as “solutions oriented” platforms where people come seeking drugs for, say, weight loss or erectile dysfunction that company providers dutifully prescribe. “They really turn the clinical model on its head,” he said. Good medical practice involves taking a history, diagnosing the patient, and then deciding on what treatment is best for the patient, he said, not starting from the treatment and asking whether the patient is right for it.
Of course, you can easily find brick-and-mortar versions of that approach to medical care — men’s health clinics peddling testosterone and penile injection therapies, for example, or clinics promoting diabetes drugs for weight loss. But the DTC model supercharges that clinical model, allowing providers to reach far more potential customers.
The system is built for throughput. As in my case, people often discover DTC telehealth websites through targeted ads promoting access to prescription medications. Unlike traditional drug advertising, which is more closely monitored by federal regulators, marketing from DTC telehealth providers often neglects to mention side effects, or promotes uses of drugs that haven’t been approved by the Food and Drug Administration.
Good medical practice involves taking a history, diagnosing the patient, and then deciding on what treatment is best for the patient, Mehrotra said, not starting from the treatment and asking whether the patient is right for it.
Once a user clicks on one of those ads, they are transported to a website where chatbots may answer questions and guide potential customers to a treatment. Artificial intelligence algorithms can tailor questions about each patient’s medical history and suggest a possible diagnosis to the provider. With electronic assistance, human clinicians can complete hundreds of e-visits daily, according to a 2019 JAMA viewpoint by Mehrotra and colleagues.
That model offers little incentive to provide referrals or other care for patients. Dubin pointed out that given normal testosterone levels, his hypothetical patient’s symptoms should have triggered further investigation for, say, uncontrolled diabetes, a mental health problem such as anxiety or depression, or alcohol or drug use. A lot of these online men’s health clinics are a “one-stop shop for a Band-Aid,” said Dubin, and aren’t invested in getting to the source of the problem.
The profit model, critics say, also presents obvious incentives for physicians to prescribe more drugs. Queer Doc founder Beal is critical of any practice, be it DTC telehealth or an in-person clinic that makes money on the medications prescribed. “If you are financially incentivized by the product you’re selling, you are going to try to sell more of it,” they said.
There’s limited data on whether telehealth sites that focus on specific ailments overprescribe, although Dubin’s paper suggests that at least some companies are offering drugs too enthusiastically.
Some recent cases also point to problems in the industry. Last year, for example, federal agencies launched investigations into DTC telehealth companies Cerebral and Done Global regarding the prescription of stimulants to treat ADHD. An investigative series in The Wall Street Journal cites current and former employees who describe corporate environments they say pressured clinicians to prescribe the drugs based on cursory appointments with little follow up.
Industry sources chalk up such cases to the work of a few bad actors, rather than inherent flaws with the clinical model. Ashley Winter told me that she followed the same medical guidelines at the DTC telehealth company Odela as when she treated patients in person. While Odela does sell the drugs its providers prescribe, that practice is no more a conflict of interest than surgeons profiting from the procedures that they recommend, she said: “You just have to be ethical.”
The DTC telehealth company Ro, which offers treatment for sexual health, fertility, hair, skin, and weight loss, has layers of safety checks, according to an email from Nicholas Samonas, the company’s associate director of communications. The company has an audit program, he said, and uses software that flags when a medication may not be appropriate for a patient.
“If you are financially incentivized by the product you’re selling, you are going to try to sell more of it.”
Samonas pointed me a company-sponsored study of 10,000 male patients, which found that men treated for erectile dysfunction through Ro experienced the same type and distribution of side effects, and discontinued medications, at about the same rate as in published studies of men receiving in-person care. Those results, published in the Journal of Urology and Research in 2020, suggest that telehealth treatment was on par with conventional care, according to Ro researchers.
However, in a 2021 study published in the American Urological Association’s Journal of Urology, a panel of experts gave Ro and Hims mixed scores on how well they adhered to the organization’s guidelines for treating erectile dysfunction. Both companies did a decent job advising patients on risks and benefits of medications, but performed poorly in other areas, notably not telling men with low testosterone that drugs such as sildenafil (Viagra) may work better when combined with testosterone therapy. Neither company prescribes testosterone.
Dubin is a huge proponent of telemedicine in general, but worries that, left unchecked, the DTC model can potentially introduce questionable medical practices to vast new audiences. “Direct-to-consumer telemedicine has a lot of room to grow,” he said. “There’s a lot of things that need to be worked out in that space to make sure that we’re providing good care.”
SO EXACTLY WHO IS MINDING these virtual combination clinic-drugstores?
The onus mostly falls on state medical boards — groups of physicians charged with monitoring other physicians. But the boards typically just respond to complaints, rather than go looking for bad actors, and disciplinary action for telehealth prescribers appears to be rare.
“The disciplinary system is just totally unresponsive and inactive,” said Rebecca Haw Allensworth, a professor at Vanderbilt Law School.
As for those ads trailing me around the internet, the FDA is responsible for ensuring that promotions for prescription drugs are truthful, balanced, and accurate, FDA press officer Charlie Kohler wrote in an email. By law, ads that refer to a prescription drug by name and make claims about what it does must include a balanced description of benefits and risks.
In practice, that doesn’t always happen. The online company Nurx ran an ad on Facebook touting the anti-aging effects of tretinoin, but neglected to list (admittedly mild) side effects such as skin irritation and increased sun sensitivity. Similarly, a RocketRx ad for sildenafil, generic Viagra, promotes the drug for erectile dysfunction, but doesn’t tell you that it can cause dizziness, headache, flushing, and stomachache as well as more serious side effects such as painful, prolonged erections, abnormal vision and a sudden loss of hearing. And a MaleMD ad doesn’t mention that the prescription finasteride in its Hairsy 3-in-1 hair growth medicine can cause testicle pain, decreased sexual desire, and an inability to have or maintain erections.
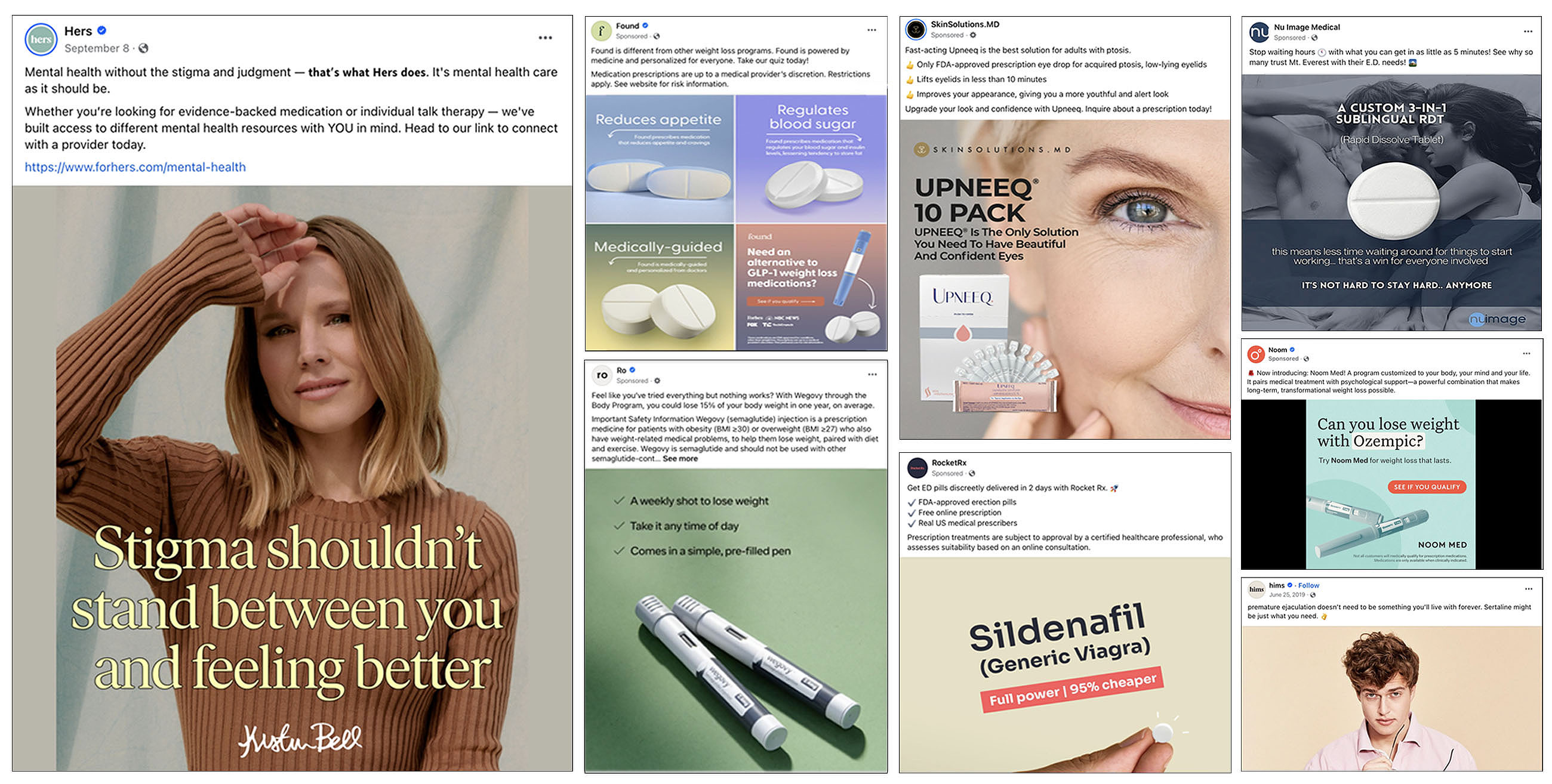
Advertisements from telehealth companies like Noom, Ro, Found, RocketRX, Hers, and even Hims, began to follow me around the internet. Image: Undark
In addition, while doctors commonly prescribe drugs for uses not approved by the FDA — beta-blockers to lessen stage fright, for example, or the diabetes drug Ozempic (semaglutide) for weight loss — the agency bans “off-label” promotion directly to consumers. But, again, DTC telehealth sites often appear to exploit a loophole allowing them to ignore those regulations.
The Hims website, for example, promotes off-label use of the antidepressant Zoloft (sertraline) for premature ejaculation. Click the “early climax” on the forhims.com home page and an animated cactus pops out of a pot, cheerily announcing: “you’re on your way to lasting longer in bed.” But despite the appeal to young men worried about their sexual performance, the site’s lengthy discussion of sertraline never says that the drug carries a black box warning — the strongest type — about the increased risk of suicidal thoughts and behaviors in teens and young adults.
In an emailed response, Hims & Hers company spokesperson Khobi Brooklyn noted that customers receive safety information on products as part of the consultation process and with prescription shipments. They also have unlimited access to health care providers to ask questions about side effects, she wrote.
Questions about the legality of the DTC telehealth ads that Kristina Bitzer saw online prompted her to dig into the topic during law school. Her analysis, published in the Northern Illinois University Law Review in 2021, found that many DTC platforms fall into a regulatory gray area defined by what they are not. The DTC companies themselves aren’t medical providers, because they contract with the professionals who provide care. They aren’t pharmaceutical companies, either, because they don’t actually make the drugs that they promote and sell. But they are also not online pharmacies, because they contract with outside companies to fill prescriptions.

During law school, Kristina Bitzer published an analysis finding that many DTC platforms fall into a regulatory gray area because they are not medical providers, pharmaceutical companies, or online pharmacies. Image: Courtesy of Kristina Bitzer
Instead, they’re middlemen who can exploit that status to market drugs online, free from government oversight.
Brooklyn confirmed that Hims & Hers does not consider itself to be a medical provider, drug maker, or pharmacy and so is not subject to FDA regulations for prescription drug marketing and promotion. “Hims & Hers connects people seeking care to independent licensed healthcare providers who work through the Hims & Hers telehealth platform,” she wrote. When asked about the specifics of purchasing and receiving a treatment, Brooklyn noted: “Prescriptions are fulfilled by one of our partner or affiliated pharmacies, who ship the product directly to customers.”
The FDA’s Kohler would not comment on specific ads, but he did acknowledge that some companies are out the agency’s purview. Social media companies, whose policies appear more lenient than federal law, have also been permissive toward DTC drug advertising. For example, Meta, the parent company of Facebook and Instagram, allows ads that “share information around medical efficacy, accessibility and affordability of different types of treatments,” company spokesperson Rachel Hamrick wrote in an email. No mention of risks is required.
In theory, DTC telehealth is a good idea, said Bitzer. The problem, she said, “is that without any kind of real governance of the system, and where these telemedicine platforms are saying, ‘Well, we don’t fit into any of that, we’re doing our own thing,’ there’s a real issue for patient safety.”
IWONDERED IF I GOT SUCKERED by ads, or if my prescription face cream was as good of a deal as it seemed like at the time. As a point of comparison, I made an appointment with a local dermatologist, who did a skin-cancer check, noted mild psoriasis on the back of my neck, and wrote me a prescription for tretinoin. The drug was cheaper at my local pharmacy, I discovered, but under my health plan I had to pay $190 out of pocket for the doctor visit. Although I got a more thorough exam in person, it was a far more expensive way to get the prescription.
In addition, the Hers cream is a nicer moisturizer. And, in any case, like many of these platforms, Hers automatically signs you up for a recurring subscription and I haven’t gotten around to cancelling.
But for many patients, the stakes are much higher. It makes sense that regulators should specifically address the DTC market.
“Until someone starts regulating this more carefully, there’s a potential for harm.”
In their JAMA Internal Medicine editorial, Woloshin and Gill called on the Federation of State Medical Boards, a nonprofit organization representing medical and osteopathic boards in U.S. states and territories, to be proactive — perhaps by encouraging state boards to periodically conduct undercover spot checks of randomly selected telehealth sites.
Whether state medical boards are willing and able to provide that kind of oversight is another question. State boards have no jurisdiction over businesses, just individual practitioners, said Lisa Robin, chief advocacy officer at the FSMB. And in the absence of a complaint, state boards don’t audit practices, said Robin. “That’s just not how the system is set up in this country.”
That traditional regulatory model has started to fall apart when it comes to DTC platforms, said Mehrotra. The company, not individual providers, decides how to create questionnaires, screen patients, and advertise products, he said. So while it seems like the company should be regulated, said Mehrotra, “we don’t have a regulatory framework for that.”

My anti-aging face cream from Hers seemed like a good deal at the time. A subsequent appointment with a dermatologist provided a cheaper option for a tretinoin cream, but the cost of the doctor visit made it an expensive way to get the prescription. Image: Teresa Carr
However, Allensworth, the law professor, is leery of imposing extra regulations on DTC platforms. Putting special limitations on where and when doctors prescribe can limit access to care, she said. “We have such a terrible health care shortage in this country,” she said. “And I just think that’s almost always going to be the wrong way to respond to it.” Medical boards do have the authority to undertake robust investigations and discipline errant telehealth providers, she pointed out. Like Woloshin and Gill, she’d like to see a national effort for the boards to do so.
As for anything-goes advertising, Bitzer suggested in her analysis that, at the very least, Congress could update laws so that telehealth platforms are subject to the same regulations as drug companies marketing and promotion.
In the near term, the FDA seems unlikely to take action. Spokesperson Charlie Kohler said that the agency doesn’t comment on future potential regulatory activity, but telehealth is not listed on any of the FDA’s agendas for this year.
In the meantime, as a minimal check on who is treating them, prospective customers can look up their provider’s credentials and disciplinary record on the FSMB-run website DocInfo.org.
Patients need to be cautious, said Woloshin. “Until someone starts regulating this more carefully,” he added, “there’s a potential for harm.”
This article was originally published on Undark. Read the original article.



