July 29, 2021 by Howard Wolinsky
In late 2010, I underwent a biopsy without much of a thought. My internist had recommended the procedure after suspecting, based on blood tests, that I was at elevated risk for prostate cancer.
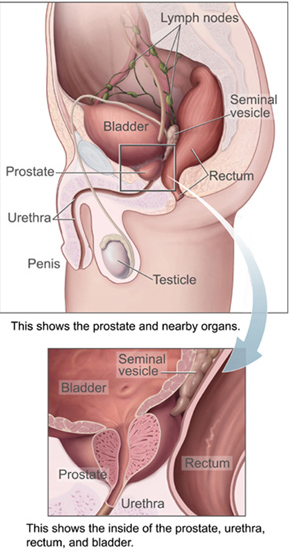
Off I went to my neighborhood urologist, who had me change into a robe, hop on an exam table, and lie on my side as he delivered numbing local anesthetic in my prostate gland, the walnut-sized organ situated between the bladder and the penis.
Over the next 10 minutes, he propelled a hollow needle from a biopsy gun through my rectum 12 times, collecting minuscule samples of my prostate with each plunge.
The procedure, known as a transrectal biopsy, has been considered the gold standard for diagnosing prostate cancer, a condition that affects roughly one in eight American men during their lifetimes.
But transrectal biopsies are also risky: They can cause infections and, on rare occasions, a life-threatening condition known as sepsis. I started writing about these risks in 2018 after a friend, a facial plastic surgeon, nearly died from a transrectal procedure at the hands of his urologist.
Concerns over these risks have led a growing number of physicians around the world to abandon the procedure, in favor of safer methods. But in the United States, most doctors still cling to the transrectal biopsy, despite the potential dangers. This must change. There are far too many lives at stake.
Nearly 250,000 men this year will be diagnosed with prostate cancer in the U.S., according to the American Cancer Society. Because prostate cancer is typically slow growing — and practically inevitable in men who live long enough — more than a third of patients diagnosed with the condition don’t undergo surgery or radiation therapy but are instead placed on active surveillance, a regimen of blood tests, digital exams, MRIs, and biopsies aimed at tracking the cancer’s growth and providing an early warning should the cancer advance.
Compared with surgery, a transrectal biopsy may seem like a harmless option. It isn’t. The rectal lining is ridden with potentially infectious bacteria, and 5 to 7 percent of patients who undergo prostate biopsies — the vast majority of which are transrectal — develop infections, according to the American Urological Association, or AUA. In up to 3 percent of transrectal biopsy cases, the infections trigger potentially life-threatening and disabling sepsis.
No one knows for sure how many people die from transrectal biopsies. But in 2019, Truls E. Bjerklund Johansen, a consultant urologist and professor emeritus at the University of Oslo, and Per‑Henrik Zahl, a senior scientist at the Norwegian Institute of Public Health in Oslo, looked into the question after one of Bjerklund Johansen’s biopsy patients died from a brain clot, likely triggered by sepsis.
The researchers concluded, based on a national patient registry, that one in every 1,000 Norwegian men who underwent a transrectal biopsy died within 30 days of the procedure. Assuming a similar trend holds in the U.S., that would translate to roughly 2,000 deaths each year, or roughly five per day, Bjerklund Johansen said.
Transrectal biopsy patients are commonly given powerful antibiotics in preemptive attempts to ward off infection, but such protections aren’t foolproof, and they are likely contributing to a rising plague of antibiotic resistant infections, which claim an estimated 35,000 lives annually in the U.S. alone.
Bjerklund Johansen is among a growing contingent of doctors who have decided that the safest way to collect prostate tissue is not through the rectum but through the perineum, the skin between the testicles and anus. Unlike the rectum, the perineum can be easily disinfected, and also has another major advantage: It can provide a clearer pathway to the anterior prostate, a region that is harder to reach with transrectal biopsies. The anterior section, the “ceiling” of the organ, is the site of 20 to 35 percent of prostate cancers.
If the transperineal biopsy is so great, why don’t all urologists switch?
One reason may be urologists underestimating the risk of transrectal biopsies. An old maxim holds that doctors bury their mistakes, and in the case of transrectal biopsies, mistakes may be hidden behind a misleading cause of death listed on death certificates. Urologists might not link a death from septic shock to transrectal biopsy, even if a biopsy was performed just days earlier. When individual doctors acknowledge the risk of post-biopsy infection, they may believe that infection rates among their own patients are low.
Perhaps more crucially, there’s little financial incentive for urologists to make the switch in the U.S. To adopt the technique, they may need to invest large sums of money in new equipment and will need to undergo training to learn a procedure that — at least initially — will be slightly more time-consuming to perform than its transrectal counterpart. Yet the reimbursements doctors receive from insurers for transperineal biopsies may be about the same as they would get for transrectal procedures.
Some research also shows the transperineal technique is slightly more painful than the traditional transrectal biopsy. Richard Szabo, an associate clinical professor in the department of urology at the University of California, Irvine, performed a literature review on the subject and found that transperineal pain scores averaged 3.17 on a 10-point scale — with 10 being the most severe pain — while transrectal pain scores averaged 2.5. But, anecdotally, men I know who have had both procedures say the pain levels are about the same.
Although the relative merits of the transperineal biopsy continue to be debated, momentum for the procedure has been growing in Europe, China, Australia, and elsewhere. In Australia, the national health plan now offers a higher reimbursement amount for transperineal procedures in an effort to make them the new standard of care. In 2017, Guy’s Hospital, a National Health Service facility in London, stopped doing transrectal biopsies altogether. By March 2019, all six of the hospitals in the South East London Cancer Network had followed suit. In January 2021, the European Association of Urology stated in a position paper that “available evidence highlights that it is time for the urological community to switch from a transrectal to a transperineal [prostate biopsy] approach despite any possible logistical challenges.”
Bjerklund Johansen said that transrectal procedures have been abandoned in most of Norway.
The U.S. has been slower to come around. Bjerklund Johansen said U.S. urologists were skeptical of his research when he presented at the 2019 annual meeting of the AUA. Matthew Allaway, a urologist who invented a device used to position the biopsy needle in transperineal procedures, estimates that only 5 percent of prostate biopsies in the U.S. are performed transperineally, though that number may be even lower. Anecdotally, he estimates that about 60 percent of urologists have switched to the transperineal approach in Britain, and that anywhere from 5 to 30 percent of them have abandoned the transrectal approach across the European Union.
The winds of change, however, may be blowing. A few American urologists — including Szabo and Allaway — have joined with like-minded experts from Europe and Australia on a campaign they describe as “TRexit,” short for transrectal exit (and a tongue-in-cheek reference to “Brexit,” the popular shorthand for Britain’s exit from the European Union). The group’s bold goal is for urologists worldwide to abandon transrectal biopsies by the end of 2022. There’s a long way to go.
What about me?
My case is a bit unusual. Although I have undergone six biopsies, all of them transrectal, doctors have detected cancerous cells only once, nearly 11 years ago. My blood tests and MRIs have come back clean.
I recognize that not everyone is so fortunate, and this year I started an underground network of sorts, that helps connect prostate cancer patients with practitioners who offer transperineal biopsies. In some cases, patients have been willing to drive more than 1,000 miles and cross state lines to avoid subjecting themselves to the unnecessary risk of a transrectal procedure.
It is time for the AUA to get its act together and join organizations like the European Association of Urology in recommending transperineal biopsies as a safer alternative to transrectal biopsies. (An AUA spokeswoman said the organization is in the early stage of developing a clinical guideline on detecting prostate cancer and is currently reviewing the benefits and harms of transrectal and transperineal biopsies as part of the guideline. The issue will be debated at the AUA’s annual meeting in Las Vegas this September.)
I told my own doctor four years ago that urologists will face a patient revolution if they don’t start addressing this issue. He said that his job was to surveil, and defended his office’s use of transrectal biopsies as a relatively low-risk method of monitoring prostate cancer.
Today, that same doctor has joined the TRexit and is planning to offer transperineal biopsies in his suburban Chicago office.
The revolution may, at last, be underway.
UPDATE: A previous version of this piece described Truls E. Bjerklund Johansen as an adjunct professor at at the University of Oslo. As of June, he is a professor emeritus. The piece also incorrectly described TRexit’s goal as eliminating transperineal biopsies by the end of 2022. The goal is to eliminate transrectal biopsies.
Howard Wolinsky is a Chicago-based freelance medical writer. He worked as a medical and science reporter for The Chicago Sun-Times and writes the “A Patient’s Journey” blog for MedPageToday.com.
This article was originally published on Undark.
Read the original article.



