This is Part One of Stateline’s 2018 Legislative Review.
By Christine Vestal, Stateline
Kentucky Republican Gov. Matt Bevin says he doesn’t want more able-bodied poor people to get Medicaid in his state unless a portion of them are required to work.
And when Republicans in Virginia agreed to expand Medicaid this year, they also said recipients who are able would have to work.
In several states this year, the march to bring health care benefits to more low-income residents came with the insistence that able-bodied adults — who are just a fraction of all Medicaid recipients — put in hours of work or volunteer time each month to retain the assistance.
The politics worked: Many Democratic lawmakers went along as assurance that more people could reap benefits from the Affordable Care Act, while Republicans were able to show their base that they were holding people accountable for receiving aid. As a result, Republican-led states have increasingly expanded coverage with such restrictions, and some red states that had already expanded Medicaid are opting to add them.
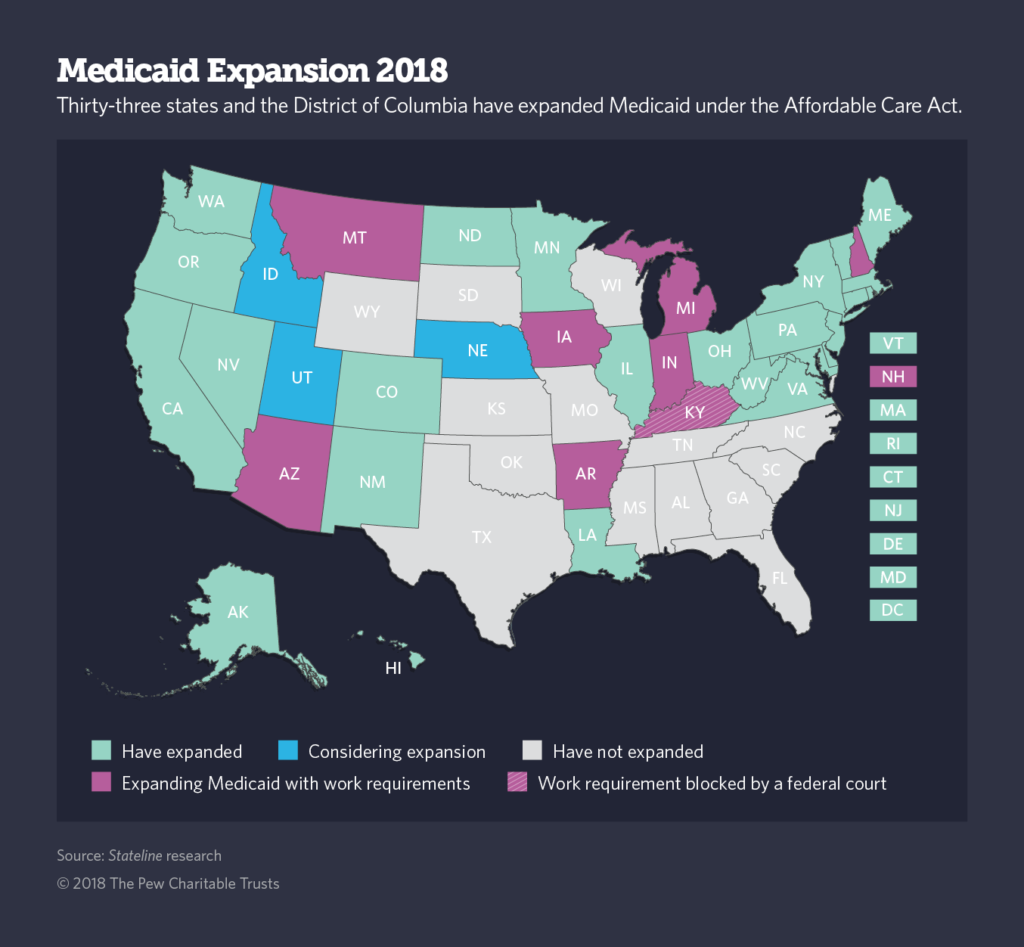
Although a court has temporarily halted Kentucky’s plan, three other expansion states – Arkansas, Indiana and New Hampshire — have federally approved work requirement waivers in place. Another three expansion states — Arizona, Ohio and Maine — are seeking permission to do the same.
Utah is considering a Medicaid expansion that would include a work requirement, and eight non-expansion states — Alabama, Kansas, Mississippi, Oklahoma, South Carolina, South Dakota, Tennessee and Wisconsin — want to require work for some traditional Medicaid recipients. North Carolina has ruled that if it decides to expand Medicaid, it would do so with a work requirement.
“If work requirements are what it takes to get conservative states to expand coverage to hundreds of thousands of people, then I’m inclined to say, ‘Let’s make it work.’” — Len Nichols, director The Center for Health Policy Research at George Mason University
According to the Kaiser Family Foundation, more than 6 in 10 adult Medicaid enrollees are already working in a variety of jobs, including retail sales, home health care, restaurants and hotels, cleaning services, transportation and customer service. And about a quarter of non-working adults would be exempt from state work requirements for health reasons or because they are caring for a child or ailing family member.
As a result, only a small share of the targeted adult Medicaid population — 6 percent — would be subject to the restriction. But, according to Kaiser and other research and advocacy groups, a much larger share of enrollees, both those who are working and those seeking exemptions, would be subject to reporting requirements and could fail to make timely filings, primarily because they do not have access to a computer. At least a third of adults in Medicaid never use a computer.
Critics argue that work requirements would cause many Americans with chronic health conditions to lose health coverage, making them less likely to ever hold down a steady long-term job. Supporters, including the Trump administration, argue that compelling Medicaid enrollees to work would spare taxpayer dollars and improve the overall well-being of those who work.
“There is a robust body of academic evidence to show that work is a key component of well-being,” Health and Human Services Secretary Alex Azar said in February when he announced approval of Indiana’s work waiver.
In the middle, some health policy experts say that work requirements and other “skin in the game” provisions, such as charging copays and small premiums or requiring enrollees to maintain health savings accounts, may be worth the potential loss of coverage if the restrictions allow political leaders in the remaining 17 states that have not expanded Medicaid to do so.
“If work requirements are what it takes to get conservative states to expand coverage to hundreds of thousands of people, then I’m inclined to say, ‘Let’s make it work,’” said Len Nichols, director of George Mason University’s Center for Health Policy Research and Ethics and a former health care adviser to President Bill Clinton.
Kentucky’s Bevin said during his 2015 campaign for governor that he’d repeal his predecessor’s decision to expand Medicaid under the Affordable Care Act to low-income adults unless at least some of them were required to work. He won federal approval to waive traditional Medicaid rules and require certain adults to work.
But a federal court decision in June blocked Kentucky’s work requirement, which was slated to take effect in July, and forced the federal government to come up with new evidence to explain how work requirements and other enrollment restrictions promote the statutory goal of the federal-state program: to provide publicly funded health insurance to uninsured, low-income Americans.
In July, the federal government announced it would seek a new round of public comment on the issue and submit a new waiver approval for Kentucky’s Medicaid program within the next two months.
In the meantime, the federal district court ruling has no direct effect on other states that are considering applying for or already have received federal approval to require work as a condition of Medicaid enrollment.
A Medicaid Experiment
Throughout Medicaid’s more than 50-year history, each state has tailored the program to meet its individual fiscal and health care needs.
Work requirements and other provisions designed to encourage people to get off the rolls are a continuation of that process, said Matt Salo, director of the National Association of Medicaid Directors.
Salo said the federal court decision puts states and the federal government on notice that if they want to bend Medicaid’s existing rules, they must come up with compelling evidence to balance state and federal aims of limiting spending on the $553 billion program against Medicaid’s overarching goal of covering low-income Americans who otherwise would lack health insurance coverage.
Kentucky’s proposal to waive existing Medicaid rules “had nothing to do with providing affordable medical assistance,” said Jane Perkins, legal director of the National Health Law Program, which represented the plaintiffs in the case. “Any time you do an experiment with Medicaid, there can be some people who would lose coverage. But Kentucky’s stated goal was to cut enrollment.”
Nationwide, as many as 4 million of the nearly 74 million people enrolled in Medicaid would lose their coverage if all states implemented work requirements similar to those proposed in Kentucky and others states, according to the Kaiser Family Foundation.
In its waiver request, for example, Kentucky wrote that requiring some of the 500,000 able-bodied adults in the state’s expanded Medicaid program to work and pay premiums and copays would lower enrollment by 95,000 over time, at a savings to the state of $331 million.
Saving taxpayer money by pushing people to increase their income and get off the rolls will help sustain the Medicaid program so that it can continue to serve the truly vulnerable, then-Secretary of Health and Human Services Tom Price wrote in a 2017 letter to governors.
When Medicaid Is Called Welfare
When Maine’s conservative Republican Gov. Paul LePage delivered his first state of the state address, in 2012, he listed “unsustainable welfare spending” among the state’s most pressing problems and asked the Legislature to approve drastic enrollment cuts to the program.
He was talking about Medicaid, but refused to use its name. To him, it was welfare.
Five years later, when a measure that would expand the program under the ACA got the required number of signatures to make the ballot, LePage insisted voters be asked to vote “yes” or “no” on expanding “welfare” — not Medicaid. He lost his battle over the wording, and the measure was approved by voters. Now he’s refusing to implement it.
“Characterizing Medicaid as welfare is simply an attempt to demean it, because of the stigma that is attached to welfare in the United States,” said Sara Rosenbaum, chairwoman of the health policy department at George Washington University.
In the Trump administration’s continuing effort to dismantle the Affordable Care Act and cut federal spending on social programs, it has lumped Medicaid with other public assistance programs such as food stamps and federal housing aid in instituting new job requirements, she said.
Some Republicans have argued that Medicaid can create a pathway to work. When he broke ranks with his party in 2013 to expand Medicaid, Ohio Gov. John Kasich said in a television news interview that people with mental illness and drug addiction are among those who need medical assistance to help them “get across the bridge so they can get employment.”
Other conservatives say that mandatory work rules may be the best way to push people into the workforce.
Nina Owcharenko Schaefer, a health policy expert at the conservative Heritage Foundation, said that the working-age, able-bodied adults who were added to Medicaid under the ACA, also known as “Obamacare,” weren’t envisioned when traditional Medicaid rules were written.
“The point is that there’s a group of people on Medicaid now, particularly in expansion states, who don’t have children and who look like they can work and probably can. The disagreement is about how you find these people.” — Robert Kaestner, economist The University of Illinois at Chicago
Already Working
Both sides in the debate over work rules point to estimates of the number of Medicaid enrollees who already are working.
According to the Kaiser Family Foundation, at least 60 percent of the nearly 25 million able-bodied adults in Medicaid are working but don’t receive health coverage from their employers or can’t afford it.
The administration’s Council of Economic Advisers reports the reverse — 60 percent of able-bodied adults enrolled in Medicaid “work few if any hours each week while receiving benefits.”
Robert Kaestner, an economist at the University of Illinois at Chicago, argued that the debate should not be about how many people in Medicaid are working.
“The point is that there’s a group of people on Medicaid now, particularly in expansion states, who don’t have children and who look like they can work and probably can,” he said. “The disagreement is about how you find these people.”
“The challenge,” he said, “is to write policy in a way that doesn’t penalize people who for various reasons shouldn’t be working.”
Work requirements in Kentucky and other states exempt people who are taking care of children and elderly or disabled adults, attending school, or receiving vocational training. Most states allow community volunteer work as a substitute for paid work.
Critics of the new rules argue that more people are likely to lose benefits because they don’t know about the requirements or are unable to fill out the paperwork to prove they are either exempt from work requirements or engaged in acceptable work activities.
In Arkansas, for example, after implementing work rules for the first time in June, the state reported that at least 7,000 people could lose coverage — most because they either didn’t know about the new requirement or couldn’t get access to a computer with internet access to fill out the forms, said Marquita Little, health policy director for Arkansas Advocates for Family and Children, which lobbied against the work rule when it was considered by the Legislature in 2017.
“It’s the law now,” Little said, “so we’re working with the community and the state to provide a continuous feedback loop so we can help more people comply and not lose coverage.”
Indiana and New Hampshire are slated to start implementing Medicaid work requirements in January 2019.
Kaiser Health News, a nonprofit health newsroom whose stories appear in news outlets nationwide, is an editorially independent part of the Kaiser Family Foundation.


