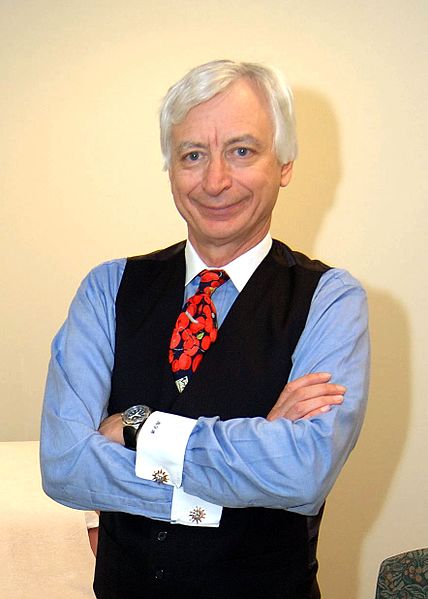
Dr. Michael Holick’s enthusiasm for vitamin D can be fairly described as extreme.
The Boston University endocrinologist, who perhaps more than anyone else is responsible for creating a billion-dollar vitamin D sales and testing juggernaut, elevates his own levels of the stuff with supplements and fortified milk. When he bikes outdoors, he won’t put sunscreen on his limbs.
He has written book-length odes to vitamin D, and has warned in multiple scholarly articles about a “vitamin D deficiency pandemic” that explains disease and suboptimal health across the world.
His fixation is so intense that it extends to the dinosaurs. What if the real problem with that asteroid 65 million years ago wasn’t a lack of food, but the weak bones that follow a lack of sunlight? “I sometimes wonder,” Holick has written, “did the dinosaurs die of rickets and osteomalacia?”
Holick’s role in drafting national vitamin D guidelines, and the embrace of his message by mainstream doctors and wellness gurus alike, have helped push supplement sales to $936 million in 2017. That’s a ninefold increase over the previous decade. Lab tests for vitamin D deficiency have spiked, too: Doctors ordered more than 10 million for Medicare patients in 2016, up 547 percent since 2007, at a cost of $365 million. About 1 in 4 adults 60 and older now take vitamin D supplements.
But few of the Americans swept up in the vitamin D craze are likely aware that the industry has sent a lot of money Holick’s way. A Kaiser Health News investigation found that he has used his prominent position in the medical community to promote practices that financially benefit corporations that have given him hundreds of thousands of dollars — including drugmakers, the indoor-tanning industry and one of the country’s largest commercial labs.
In an interview, Holick acknowledged he has worked as a consultant to Quest Diagnostics, which performs vitamin D tests, since 1979. Holick, 72, said that industry funding “doesn’t influence me in terms of talking about the health benefits of vitamin D.”
There is no question that the hormone is important. Without enough of it, bones can become thin, brittle and misshapen, causing a condition called rickets in children and osteomalacia in adults. The issue is how much vitamin D is healthy, and what level constitutes deficiency.
Holick’s crucial role in shaping that debate occurred in 2011. Late the previous year, the prestigious National Academy of Medicine (then known as the Institute of Medicine), a group of independent scientific experts, issued a comprehensive, 1,132-page report on vitamin D deficiency. It concluded that the vast majority of Americans get plenty of the hormone through diet and sunlight, and advised doctors to test only patients at high risk of vitamin D-related disorders, such as osteoporosis.
A few months later, in June 2011, Holick oversaw the publication of a report that took a starkly different view. The paper, in the peer-reviewed Journal of Clinical Endocrinology & Metabolism, was on behalf of the Endocrine Society, the field’s foremost professional group, whose guidelines are widely used by hospitals, physicians and commercial labs nationwide, including Quest. The society adopted Holick’s position that “vitamin D deficiency is very common in all age groups” and advocated a huge expansion of vitamin D testing, targeting more than half the United States population, including those who are black, Hispanic or obese — groups that tend to have lower vitamin D levels than others.
The recommendations were a financial windfall for the vitamin D industry. By advocating such widespread testing, the Endocrine Society directed more business to Quest and other commercial labs. Vitamin D tests are now the fifth-most-common lab test covered by Medicare.
The guidelines benefited the vitamin D industry in another important way. Unlike the National Academy, which concluded that patients have sufficient vitamin D when their blood levels are at or above 20 nanograms per milliliter, the Endocrine Society said vitamin D levels need to be much higher — at least 30 nanograms per milliliter. Many commercial labs, including Quest and LabCorp, adopted the higher standard.
Yet there’s no evidence that people with the higher level are any healthier than those with the lower level, said Dr. Clifford Rosen, a senior scientist at the Maine Medical Center Research Institute and co-author of the National Academy report. Using the Endocrine Society’s higher standard creates the appearance of an epidemic, he said, because it labels 80 percent of Americans as having inadequate vitamin D.
“We see people being tested all the time and being treated based on a lot of wishful thinking, that you can take a supplement to be healthier,” Rosen said.
Patients with low vitamin D levels are often prescribed supplements and instructed to get checked again in a few months, said Dr. Alex Krist, a family physician and vice chairman of the U.S. Preventive Services Task Force, an expert panel that issues health advice. Many physicians then repeat the test once a year. For labs, “it’s in their financial interest” to label patients with low vitamin D levels, Krist said.
In a 2010 book, “The Vitamin D Solution,” Holick gave readers tips to encourage them to get their blood tested. For readers worried about potential out-of-pocket costs for vitamin D tests — they range from $40 to $225 — Holick listed the precise reimbursement codes that doctors should use when requesting insurance coverage. “If they use the wrong coding when submitting the claim to the insurance company, they won’t get reimbursed and you will wind up having to pay for the test,” Holick wrote.
Holick acknowledged financial ties with Quest and other companies in the financial disclosure statement published with the Endocrine Society guidelines. In an interview, he said that working for Quest for four decades — he is currently paid $1,000 a month — hasn’t affected his medical advice. “I don’t get any additional money if they sell one test or 1 billion,” Holick said.
A Quest spokeswoman, Wendy Bost, said the company seeks the advice of a number of expert consultants. “We feel strongly that being able to work with the top experts in the field, whether it’s vitamin D or another area, translates to better quality and better information, both for our patients and physicians,” Bost said.
Since 2011, Holick’s advocacy has been embraced by the wellness-industrial complex. Gwyneth Paltrow’s website, Goop, cites his writing. Dr. Mehmet Oz has described vitamin D as “the No. 1 thing you need more of,” telling his audience that it can help them avoid heart disease, depression, weight gain, memory loss and cancer. And Oprah Winfrey’s website tells readers that “knowing your vitamin D levels might save your life.” Mainstream doctors have pushed the hormone, including Dr. Walter Willett, a widely respected professor at Harvard Medical School.
Today, seven years after the dueling academic findings, the leaders of the National Academy report are struggling to be heard above the clamor for more sunshine pills.
“There isn’t a ‘pandemic,’” A. Catharine Ross, a professor at Penn State and chair of the committee that wrote the report, said in an interview. “There isn’t a widespread problem.”
Ties To Drugmakers And Tanning Salons
In “The Vitamin D Solution,” Holick describes his promotion of vitamin D as a lonely crusade. “Drug companies can sell fear,” he writes, “but they can’t sell sunlight, so there’s no promotion of the sun’s health benefits.”
Yet Holick also has extensive financial ties to the pharmaceutical industry. He received nearly $163,000 from 2013 to 2017 from pharmaceutical companies, according to Medicare’s Open Payments database, which tracks payments from drug and device manufacturers. The companies paying him included Sanofi-Aventis, which markets vitamin D supplements; Shire, which makes drugs for hormonal disorders that are given with vitamin D; Amgen, which makes an osteoporosis treatment; and Roche Diagnostics and Quidel Corp., which both make vitamin D tests.
The database includes only payments made since 2013, but Holick’s record of being compensated by drug companies started before that. In his 2010 book, he describes visiting South Africa to give “talks for a pharmaceutical company,” whose president and chief executive were in the audience.
Holick’s ties to the tanning industry also have drawn scrutiny. Although Holick said he doesn’t advocate tanning, he has described tanning beds as a “recommended source” of vitamin D “when used in moderation.”
Holick has acknowledged accepting research money from the UV Foundation — a nonprofit arm of the now-defunct Indoor Tanning Association — which gave $150,000 to Boston University from 2004 to 2006, earmarked for Holick’s research. The International Agency for Research on Cancer classified tanning beds as carcinogenic in 2009.
In 2004, the tanning-industry associations led Dr. Barbara Gilchrest, who then was head of Boston University’s dermatology department, to ask Holick to resign from the department. He did so, but remains a professor at the medical school’s department of endocrinology, diabetes and nutrition and weight management.
In “The Vitamin D Solution,” Holick wrote that he was “forced” to give up his position due to his “stalwart support of sensible sun exposure.” He added, “Shame on me for challenging one of the dogmas of dermatology.”
Although Holick’s website lists him as a member of the American Academy of Dermatology, an academy spokeswoman, Amanda Jacobs, said he was not a current member.
Dr. Christopher McCartney, chairman of the Endocrine Society’s clinical guidelines subcommittee, said the society has put in place stricter policies on conflict of interest since its vitamin D guidelines were released. The society’s current policies would not allow the chairman of the guideline-writing committee to have financial conflicts.
A Miracle Pill Loses Its Luster
Enthusiasm for vitamin D among medical experts has dimmed in recent years, as rigorous clinical trials have failed to confirm the benefits suggested by early, preliminary studies. A string of trials found no evidence that vitamin D reduces the risk of cancer, heart disease or falls in the elderly. And most scientists say there isn’t enough evidence to know if vitamin D can prevent chronic diseases that aren’t related to bones.
Although the amount of vitamin D in a typical daily supplement is generally considered safe, it is possible to take too much. In 2015, an article in the American Journal of Medicine linked blood levels as low as 50 nanograms per milliliter with an increased risk of death.
Some researchers say vitamin D may never have been the miracle pill that it appeared to be. Sick people who stay indoors tend to have low vitamin D levels; their poor health is likely the cause of their low vitamin D levels, not the other way around, said Dr. JoAnn Manson, chief of preventive medicine at Brigham and Women’s Hospital in Boston. Only really rigorous studies, which randomly assign some patients to take vitamin D and others to take placebos, can provide definitive answers about vitamin D and health. Manson is leading one such study, involving 26,000 adults, expected to be published in November.
A number of insurers and health experts have begun to view widespread vitamin D testing as unnecessary and expensive. In 2014, the U.S. Preventive Services Task Force said there wasn’t enough evidence to recommend for or against routine vitamin D screening. In April, the task force explicitly recommended that older adults outside of nursing homes avoid taking vitamin D supplements to prevent falls.
In 2015, Excellus BlueCross BlueShield published an analysis highlighting the overuse of vitamin D tests. In 2014, the insurer spent $33 million on 641,000 vitamin D tests. “That’s an astronomical amount of money,” said Dr. Richard Lockwood, Excellus’ vice president and chief medical officer for utilization management. More than 40 percent of Excellus patients tested had no medical reason to be screened.
In spite of Excellus’ efforts to rein in the tests, vitamin D usage has remained high, Lockwood said. “It’s very hard to change habits,” he said, adding: “The medical community is not much different than the rest of the world, and we get into fads.”
KHN’s coverage related to aging and improving care of older adults is supported in part by The John A. Hartford Foundation.
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.

