By Judith Graham, Kaiser Health News
Davetta Brooks, 75, who has heart failure, a fractured hip and macular degeneration, is afraid. Conditions in her low-income senior building on Chicago’s Near West Side — the Congressman George W. Collins Apartments — are “deplorable,” she said.
Residents are not wearing masks or gloves to guard against the coronavirus, she said: “They’re touching everything on the elevator, in the laundry room. And anybody and everybody’s relatives and friends are coming in and out with no scrutiny.”
No one is checking on residents to see if they need help, Brooks said. And no one seems to know whether residents have tested positive for COVID-19 or died, though ambulances have screeched up to the entrance several times.
“This building is not safe,” she said in mid-June. “With all the things happening in the U.S., this is what ‘seniors lives don’t matter’ looks like.”
Nationwide, more than 1.6 million older adults live in low-income housing subsidized by the Department of Housing and Urban Development — most in apartment buildings with shared common spaces, elevators, staircases, mailrooms, hallways and laundry rooms where the coronavirus might lurk.
Most of these seniors have endured a life of disadvantage, have chronic illnesses such as diabetes and heart disease, and lack financial reserves to draw upon.
Yet in the midst of the pandemic, this population — the age group deemed most at risk of becoming critically ill and dying — has largely been overlooked.
“This is a moment when we really should be pushing assistance and guidance toward these senior communities, but we’re not,” said Linda Couch, vice president of housing for LeadingAge, an association that represents nonprofit senior housing and long-term care providers. “No one is watching over what’s happening.”
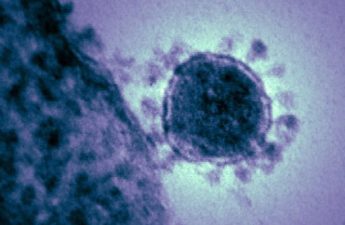
Nationally there is no data on COVID-19’s spread in low-income housing. The Centers for Disease Control and Prevention is not collecting it or requiring states to do so. The same is true of HUD and state and local housing agencies: This is “independent living,” and operators are not expected to monitor the health of residents.
Low-income housing operators find out about COVID cases only when residents or family members volunteer the information. For the most part, systematic testing is not done. A rare exception: Gov. Andrew Cuomo in mid-May announced plans to bring coronavirus testing to 40 public housing developments in New York.
“Without testing, there’s no way of knowing how many people have the virus,” said Michael Kane, executive director of the National Alliance of HUD Tenants. “Our concern is that there could be a transmission danger similar to what’s going on in nursing homes or assisted living.”
“People are dying all over in these buildings, and we don’t know what they’re dying from,” said Geraldine Collins, president of the National Alliance of HUD Tenants.
The situation in Chicago highlights how difficult it is to gauge the extent to which people in these settings are at risk. Although the Chicago health department requires “congregate living facilities,” including senior housing complexes, to report two or more confirmed COVID cases that occur within 14 days, it has not made that data publicly available. So there is no way of tracking where the virus is spreading.
The Chicago Housing Authority, which operates 55 buildings with 9,500 senior residents, “is not required to track or verify cases and, due to privacy issues, we do not inquire about the health status of residents,” the agency said in a statement.
At the federal level, HUD’s emergency preparedness plans did not incorporate infectious disease control and its guidance to housing operators was spotty in the pandemic’s early stages. Building managers were not required to notify residents of a COVID case.
Recently, HUD has come out more strongly on the side of transparency. On May 21, HUD said that multifamily housing management should, “in coordination with local health officials, communicate the possible COVID-19 exposure to all residents and workers, volunteers and visitors.”
On health concerns, HUD has deferred to the Centers for Disease Control and Prevention, which in March issued recommendations for preventing the spread of COVID-19 in retirement communities and independent living facilities.
Those include canceling group activities; informing residents, workers and visitors about COVID-19; stepping up cleaning and disinfecting; screening people coming into buildings; and limiting visitors.
Very little of that was happening in Chicago buildings for low-income seniors, according to Lori Clark, executive director of the Jane Addams Senior Caucus, which has close to 700 members.
When the organization called members in mid-March, “we started to hear awful stories,” Clark said. Residents reported getting no information about how to stay safe. No one was checking who was going in and out. Buildings were understaffed as workers stayed home.
At the Elizabeth Woods Apartments, a senior building operated by the Chicago Housing Authority, “we felt abandoned,” said Carmen Betances, 68. “They did no cleaning, and they did not prepare the property for the invisible enemy that has now taken over. They gave us no information about what to do.”
“I am a target for coronavirus: I am a senior. I’m asthmatic. I have a compromised immune system,” Betances said. “Every breath I take, I take with fear, worrying that I could die from this invisible monster.”
At the end of March, Betances and other residents began using their own cleaning supplies to disinfect the handles of every door in the six-story apartment building twice a day. They wiped down water fountains, counters in the lobby, chairs and tables in the community room as well as vending and laundry machines.
On May 20, the housing authority said in a statement it is making more than 3,000 calls daily to check in on older residents, requiring property management firms to clean and disinfect common areas three times a day, and distributing information about Chicago’s six new coronavirus testing sites.
The complex where Brooks lives is privately operated. Its operations were taken over April 1 by WinnResidential, the nation’s largest manager of affordable housing.
“The immediate priority during this transition has been to protect the health and safety of the residents,” wrote Ed Cafasso, senior vice president of WinnCompanies, which owns WinnResidential. He said the complex was now being cleaned several times a day.
Cafasso said the company has helped tens of thousands of older residents at 520 properties obtain meals, groceries, household supplies and masks; renew prescriptions; and access telehealth.
Food assistance is a pressing need, because people cannot get hot meals at community centers and many are afraid to go to grocery stores.
Also needed: help using technology, and better internet connections so seniors can participate in telehealth and virtual interactions with friends and family, easing their loneliness as stay-at-home orders remain in place. Most federally subsidized senior housing lacks building-wide Wi-Fi.
Going into the pandemic, some housing operators were better equipped to respond. In and around New York City, Selfhelp Community Services runs 11 low-income senior buildings with 1,400 residents. Social workers have identified vulnerable residents at the buildings and have stayed in contact with them, said Mohini Mishra, a management director.
“If someone is coming home from the hospital, we try to check in with family members,” Mishra said. “Will they need home care? Do they understand what self-quarantine means?”
Across seven of Selfhelp’s buildings, there had been 20 confirmed cases of COVID-19 among residents and 12 people had died as of June 10.
At the Paul G. Stewart Center apartments in Chicago, officials called in the police after the first resident found to have COVID-19 in mid-March refused to stay in their apartment.
“We reiterated the guidelines of the CDC and the Chicago and Illinois health department[s],” said Shawn Person, chief operations officer of the South Side campus, which houses about 1,300 residents. “But this person refused to listen. We had to do something.” As of June 10, she said, 10 residents had tested positive and two had passed away.
The complex is participating in a federal pilot project that brings nurses into senior housing to help evaluate residents’ needs.
But there’s only so much they can do. “There’s a store in this building, and nobody practices true social distancing there,” said Shirley Moore, 71, who lives in an apartment tower on the campus, has COVID-19 and is not sure how she became infected.
Her 72-year-old husband has a much worse case of COVID-19 than she does, she said. He had been in intensive care for three weeks as of June 10, including eight days on a ventilator, she said, and early on doctors told her they did not think he would survive.
“You go up in the elevators, you’re bringing garbage to the garbage chute, you’re grabbing a guardrail in the hall,” she said. “Even if there’s been cleaning, people still will be touching all these places in between.”
As for what she would like to see happen, Moore said, “I think they should be testing. I’m sure if you tested everyone in this building, you’d come up with a lot of COVID-19.”