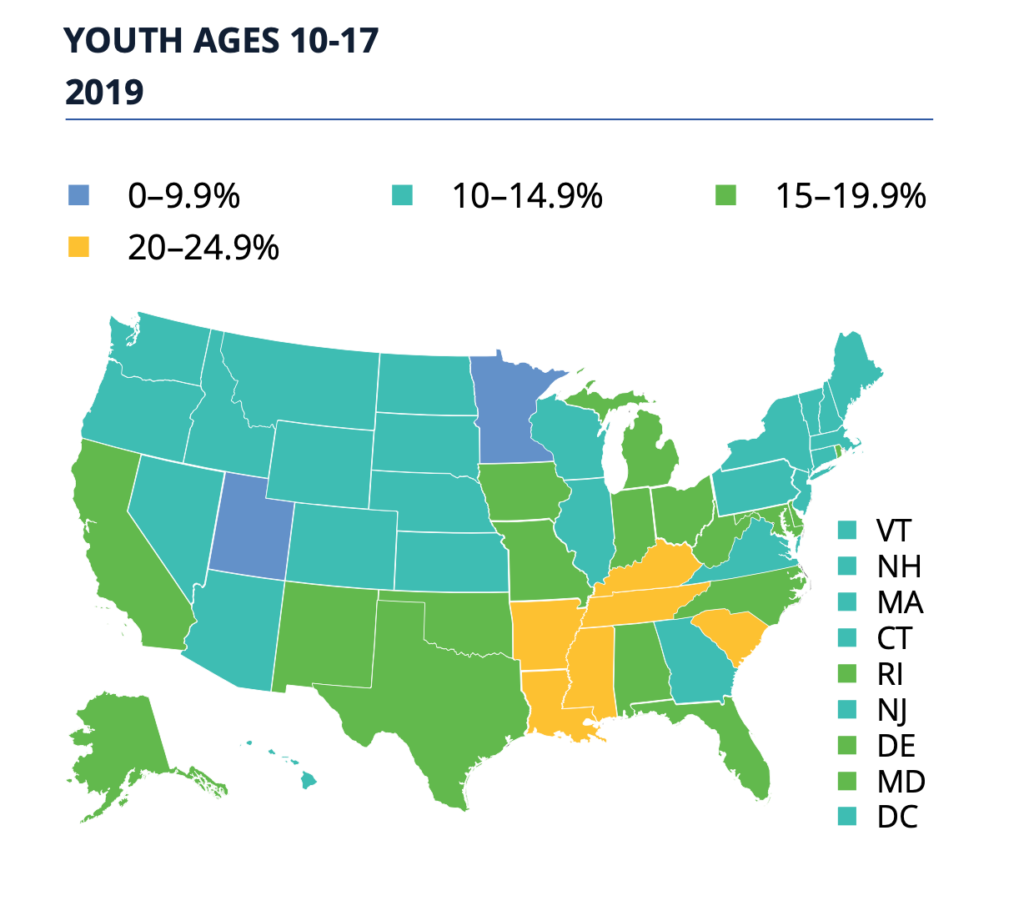
Roughly one in seven U.S. youth ages 10-17, 15.5 percent, are obese according to a new report from the Robert Wood Johnson Foundation, State of Childhood Obesity: Prioritizing Children’s Health During the Pandemic.
The report examines the latest national and state-by-state data on childhood obesity rates and offers policy recommendations for prioritizing children’s health throughout recovery.
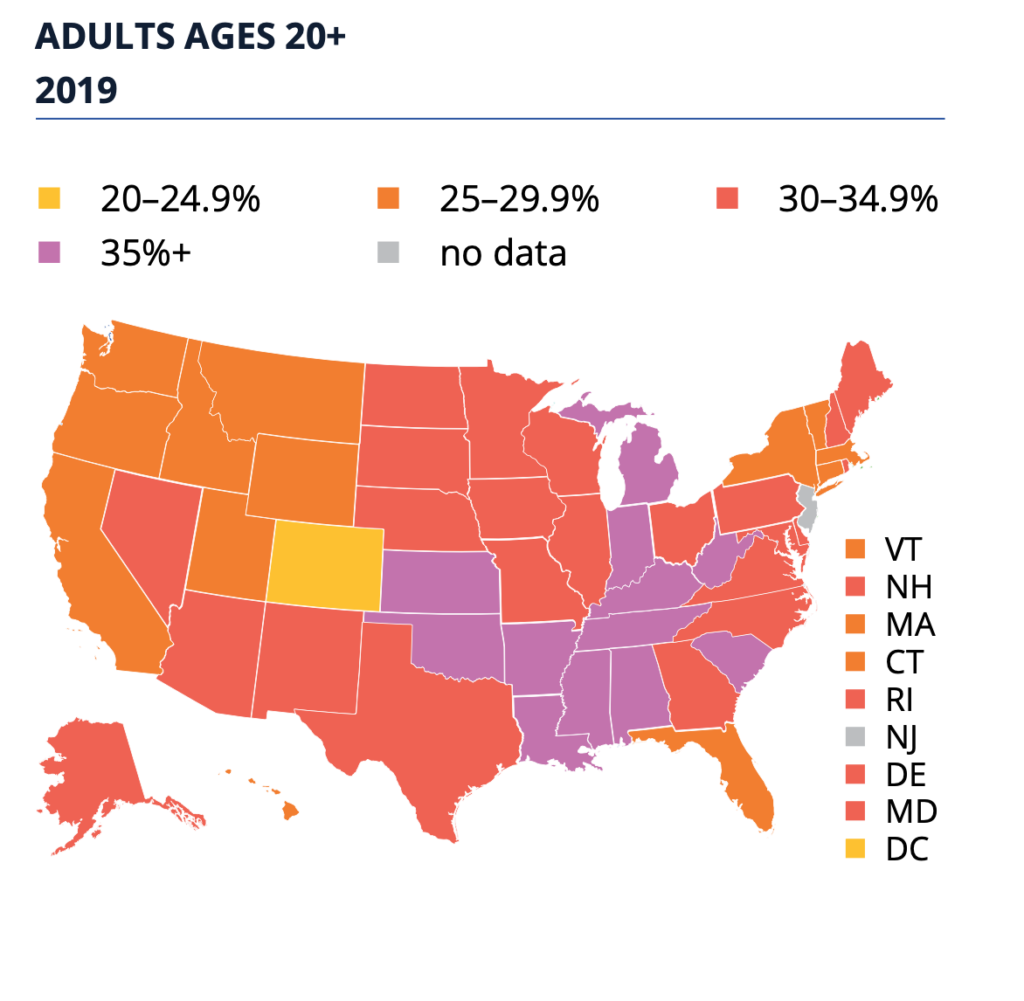
Rates among youth age 10-17 in Washington state was 11.9 percent, among adults over 20, 28.3 percent.
Key Findings from New Obesity Rate Data
● The national obesity rate for youth ages 10 to 17 in 2018-19 was 15.5 percent. The rate has held steady in recent years, though more years of data are needed to reliably assess trends over time.
● Racial and ethnic disparities persist. In 2018-2019, non-Hispanic Asian children had the lowest obesity rate (5.9%) followed by non-Hispanic white children and non-Hispanic multiple race children (11.7% and 14.7%, respectively). Obesity rates were significantly higher for Hispanic (20.7%), non-Hispanic Black (22.9%), non-Hispanic American Indian/Alaska Native (28.5%), and non-Hispanic Native Hawaiian/Other Pacific Islander (39.8%) children.
● There are also disparities by income level: 21.5 percent of youth in households making less than the federal poverty level had obesity, more than double the 8.8 percent of youth in households making at least 400 percent of the federal poverty level.
● Kentucky had the highest overall youth obesity rate, 23.8 percent, and Utah had the lowest, 9.6 percent.
● Five states had obesity rates that were statistically significantly higher than the national rate in 2018-19: Kentucky (23.8%), Mississippi (22.3%), South Carolina (22.1%), Tennessee (20.4%), and Arkansas (20.2%).
● Eight states had obesity rates that were statistically significantly lower than the national rate in 2018-19: Utah (9.6%), Minnesota (9.9%), Kansas (10.6%), Montana (10.6%), New York (10.7%), Colorado (10.9%), Hawaii (11.1%) and Nebraska (11.5%).
The data come from the combined 2018-19 National Survey of Children’s Health (NSCH), along with analysis conducted by the Health Resources and Services Administration’s Maternal and Child Health Bureau.
Implications
COVID-19
The nation’s obesity crisis and the COVID-19 pandemic intersect in many ways. Emerging research links obesity with increased risk of severe illness from COVID-19, including among children.
Evidence from other vaccines leads some to predict that a COVID-19 vaccine may be less effective among those with underlying medical conditions, including obesity.
The pandemic also exacerbates conditions that put children at risk for obesity. School closures leave millions of children without a regular source of healthy meals or physical activity. And millions of caregivers have lost income or jobs, making it more difficult for families to access or afford healthy foods.
“Childhood obesity remains an epidemic in this country,” said Jamie Bussel, senior program officer at the Robert Wood Johnson Foundation who leads the Foundation’s efforts to prevent childhood obesity. “The COVID-19 pandemic and ongoing economic recession have worsened many of the broader factors we know contribute to obesity, including poverty and health disparities. We must confront these current crises in ways that also support long-term health and equity for all children and families in the United States.”
Disparate effects
The new obesity rate data published today show that racial, ethnic, and economic disparities persist. Black, Hispanic, and Native American children have significantly higher obesity rates than White or Asian children. Young people in households making less than the federal poverty level are more than twice as likely to have obesity as those at the top of the income ladder.
“We’ve seen these disparities for decades when it comes to childhood obesity rates,” said Bussel. “This year, we’ve also seen people of color and people with low incomes hit hardest by the COVID-19 pandemic. In both cases these outcomes reflect decades of disinvestment in specific communities and specific groups of people, often driven by the systemic racism and discrimination that are still so prevalent in our society.”
Policy Recommendations
The new report highlights how key federal nutrition policies have been impacted by COVID-19 relief legislation, and makes recommendations for further changes to support health and prevent childhood obesity.
In response to the pandemic, Congress provided additional funding to the Supplemental Nutrition Assistance Program (SNAP), sometimes called food stamps. The funding was intended to help account for a jump in enrollment, which surged by nearly 6 million in the first month of the pandemic, but not to necessarily increase the benefit amount for individuals.
Recommendation: Raise the maximum SNAP benefit level by at least 15 percent per participant for the duration of the economic downturn.
The Special Supplemental Nutrition Program for Women, Infants, and Children, or WIC, has been able to change some of the ways it operates in order to support families safely. Those flexibilities nearly expired in September but were recently extended.
Recommendation: The U.S. Department of Agriculture (USDA) and Congress should ensure that the relevant waivers remain in place for as long as needed and that states and WIC offices have the technical support they need to continue to serve families.
School meal programs faced unprecedented demand in the spring, and were granted flexibility to serve meals to students outside of school. Many school districts responded by not just feeding their students but their entire communities.
Recommendation: USDA should support states in using existing waivers to serve free meals to all students through the 2020-21 school year, as recently authorized by Congress.
“SNAP, WIC, and school meals all have proven benefits for children and families,” said Bussel. “Given the unprecedented circumstances families are facing, we must make sure that they reach everyone who is eligible. Doing so will help make sure children and families can stay healthy during this pandemic, and likely reduce the risk for obesity in the long term.”