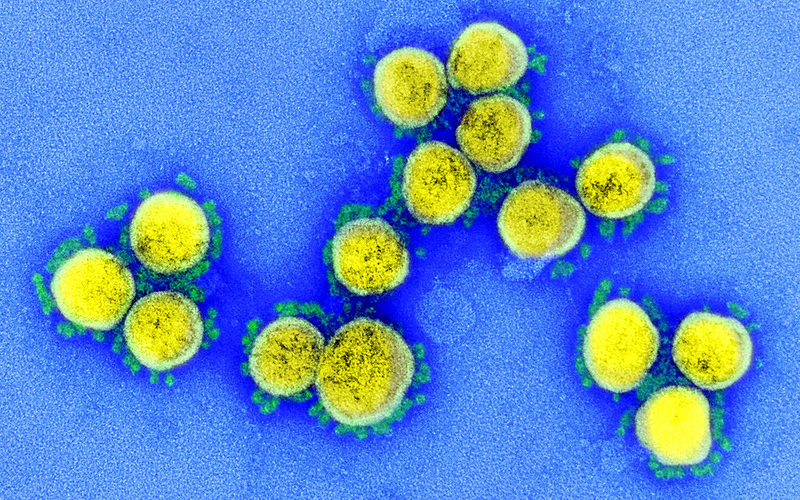
Transmission electron micrograph of SARS-CoV-2 virus particles, Credit: NIAID
Arthur Allen November, Kaiser Health News
When he started researching a troublesome childhood infection nearly four decades ago, virologist Dr. Barney Graham, then at Vanderbilt University, had no inkling his federally funded work might be key to deliverance from a global pandemic.
Yet nearly all the vaccines advancing toward possible FDA approval this fall or winter are based on a design developed by Graham and his colleagues, a concept that emerged from a scientific quest to understand a disastrous 1966 vaccine trial.
Basic research conducted by Graham and others at the National Institutes of Health, Defense Department and federally funded academic laboratories has been the essential ingredient in the rapid development of vaccines in response to COVID-19. The government has poured an additional $10.5 billion into vaccine companies since the pandemic began to accelerate the delivery of their products.
The Moderna vaccine, whose remarkable effectiveness in a late-stage trial was announced Monday morning, emerged directly out of a partnership between Moderna and Graham’s NIH laboratory.
Coronavirus vaccines are likely to be worth billions to the drug industry if they prove safe and effective. As many as 14 billion vaccines would be required to immunize everyone in the world against COVID-19. If, as many scientists anticipate, vaccine-produced immunity wanes, billions more doses could be sold as booster shots in years to come. And the technology and production laboratories seeded with the help of all this federal largesse could give rise to other profitable vaccines and drugs.
The vaccines made by Pfizer and Moderna, which are likely to be the first to win FDA approval, in particular rely heavily on two fundamental discoveries that emerged from federally funded research: the viral protein designed by Graham and his colleagues, and the concept of RNA modification, first developed by Drew Weissman and Katalin Karikó at the University of Pennsylvania. In fact, Moderna’s founders in 2010 named the company after this concept: “Modified” + “RNA” = Moderna, according to co-founder Robert Langer.
“This is the people’s vaccine,” said corporate critic Peter Maybarduk, director of Public Citizen’s Access to Medicines program. “Federal scientists helped invent it and taxpayers are funding its development. … It should belong to humanity.”
Moderna, through spokesperson Ray Jordan, acknowledged its partnership with NIH throughout the COVID-19 development process and earlier. Pfizer spokesperson Jerica Pitts noted the company had not received development and manufacturing support from the U.S. government, unlike Moderna and other companies.
The idea of creating a vaccine with messenger RNA, or mRNA — the substance that converts DNA into proteins — goes back decades. Early efforts to create mRNA vaccines failed, however, because the raw RNA was destroyed before it could generate the desired response. Our innate immune systems evolved to kill RNA strands because that’s what many viruses are.
Karikó came up with the idea of modifying the elements of RNA to enable it to slip past the immune system undetected. The modifications she and Weissman developed allowed RNA to become a promising delivery system for both vaccines and drugs. To be sure, their work was enhanced by scientists at Moderna, BioNTech and other laboratories over the past decade.
Another key element in the mRNA vaccine is the lipid nanoparticle — a tiny, ingeniously designed bit of fat that encloses the RNA in a sort of invisibility cloak, ferrying it safely through the blood and into cells and then dissolving, thereby allowing the RNA to do its work of coding a protein that will serve as the vaccine’s main active ingredient. The idea of enclosing drugs or vaccines in lipid nanoparticles arose first in the 1960s and was developed by Langer and others at the Massachusetts Institute of Technology and various academic and industry laboratories.
Karikó began investigating RNA in 1978 in her native Hungary and wrote her first NIH grant proposal to use mRNA as a therapeutic in 1989. She and Weissman achieved successes starting in 2004, but the path to recognition was often discouraging.
“I keep writing and doing experiments, things are getting better and better, but I never get any money for the work,” she recalled in an interview. “The critics said it will never be a drug. When I did these discoveries, my salary was lower than the technicians working next to me.”
Eventually, the University of Pennsylvania sublicensed the patent to Cellscript, a biotech company in Wisconsin, much to the dismay of Weissman and Karikó, who had started their own company to try to commercialize the discovery. Moderna and BioNTech later would each pay $75 million to Cellscript for the RNA modification patent, Karikó said. Though unhappy with her treatment at Penn, she remained there until 2013 — partly because her daughter, Susan Francia, was making a name for herself on the school’s rowing team. Francia would go on to win two Olympic gold medals in the sport. Karikó is now a senior officer at BioNTech.
In addition to RNA modification and the lipid nanoparticle, the third key contribution to the mRNA vaccines — as well as those made by Novavax, Sanofi and Johnson & Johnson —- is the bioengineered protein developed by Graham and his collaborators. It has proved in tests so far to elicit an immune response that could prevent the virus from causing infections and disease.
The protein design was based on the observation that so-called fusion proteins — the pieces of the virus that enable it to invade a cell — are shape-shifters, presenting different surfaces to the immune system after the virus fuses with and infects cells. Graham and his colleagues learned that antibodies against the post-fusion protein are far less effective at stopping an infection.
The discovery arose in part through Graham’s studies of a 54-year-old tragedy — the failed 1966 trial of an NIH vaccine against respiratory syncytial virus, or RSV. In a clinical trial, not only did that vaccine fail to protect against the common childhood disease, but most of the 21 children who received it were hospitalized with acute allergic reactions, and two died.
About a decade ago, Graham, now deputy director of NIH’s Vaccine Research Center, took a new stab at the RSV problem with a postdoctoral fellow, Jason McLellan. After isolating and obtaining three-dimensional models of the RSV’s fusion protein, they worked with Chinese scientists to identify an appropriate neutralizing antibody against it.
“We were sitting in Xiamen, China, when Jason got the first image up on his laptop, and I was like, oh my God, it’s coming together,” Graham recalled. The prefusion antibodies they discovered were 16 times more potent than the post-fusion form contained in the faulty 1960s vaccine.
Two 2013 papers the team published in Science earned them a runner-up prize in the prestigious journal’s Breakthrough of the Year award. Their papers, which showed it was possible to plan and create a vaccine at the microscopic structural level, set the NIH’s Vaccine Research Center on a path toward creating a generalizable, rapid way to design vaccines against emerging pandemic viruses, Graham said.
In 2016, Graham, McLellan and other scientists, including Andrew Ward at the Scripps Research Institute, advanced their concept further by publishing the prefusion structure of a coronavirus that causes the common cold and a patent was filed for its design by NIH, Scripps and Dartmouth — where McLellan had set up his own lab. NIH and the University of Texas — where McLellan now works — filed an additional patent this year for a similar design change in the virus that causes COVID-19.
Graham’s NIH lab, meanwhile, had started working with Moderna in 2017 to design a rapid manufacturing system for vaccines. In January, they were preparing a demonstration project, a clinical trial to test whether Graham’s protein design and Moderna’s mRNA platform could be used to create a vaccine against Nipah, a deadly virus spread by bats in Asia.
Their plans changed rapidly when they learned on Jan. 7 that the epidemic of respiratory disease in China was being caused by a coronavirus.
“We agreed immediately that the demonstration project would focus on this virus” instead of Nipah, Graham said. Moderna produced a vaccine within six weeks. The first patient was vaccinated in an NIH-led clinical study on March 16; early results from Moderna’s 30,000-volunteer late-stage trial showed it was nearly 95% effective at preventing COVID-19.
Although other scientists have advanced proposals for what may be even more potent vaccine antigens, Graham is confident that carefully designed vaccines using nucleic acids like RNA reflect the future of new vaccines. Already, two major drug companies are doing advanced clinical trials for RSV vaccines based on the designs his lab discovered, he said.
In a larger sense, the pandemic could be the event that paves the way for better, perhaps cheaper and more plentiful vaccines.
“It’s a silver lining, but I think we are definitely pushing forward the way everyone is thinking about vaccines,” said Michael Farzan, chair of the department of immunology and microbiology at Scripps Research’s Florida campus. “Certain techniques that have been waiting in the wings, under development but never achieving the kind of funding they needed for major tests, will finally get their chance to shine.”
Under a 1980 law, the NIH will obtain no money from the coronavirus vaccine patent. How much money will eventually go to the discoverers or their institutions isn’t clear. Any existing licensing agreements haven’t been publicized; patent disputes among some of the companies will likely last years. HHS’ big contracts with the vaccine companies are not transparent, and Freedom of Information Act requests have been slow-walked and heavily redacted, said Duke University law professor Arti Rai.
Some basic scientists involved in the enterprise seem to accept the potentially lopsided financial rewards.
“Having public-private partnerships is how things get done,” Graham said. “During this crisis, everything is focused on how can we do the best we can as fast as we can for the public health. All this other stuff is going to have to be figured out later.”
“It’s not a good look to become extremely wealthy off a pandemic,” McLellan said, noting the big stock sales by some vaccine company executives after they received hundreds of millions of dollars in government assistance. Still, “the companies should be able to make some money.”
For Graham, the lesson of the coronavirus vaccine response is that a few billion dollars a year spent on additional basic research could prevent a thousand times as much loss in death, illness and economic destruction.
“Basic research informs what we do, and planning and preparedness can make such a difference in how we get ahead of these epidemics,” he said.
“Basic research informs what we do, and planning and preparedness can make such a difference in how we get ahead of these epidemics,” he said.
This KHN story first published on California Healthline, a service of the California Health Care Foundation.
Kaiser Health News (KHN) is a national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation which is not affiliated with Kaiser Permanente.