By Michael Ollove and Christine Vestal
Stateline
Like public health officials everywhere, Dr. Jeffrey Duchin, head of public health in Seattle and King County, Washington, marvels at the miraculous production of highly effective vaccines against COVID-19 in mere months.
But Duchin, doesn’t dwell on the only triumph of the pandemic response. Instead, he quickly pivots to the huge deficiencies plaguing the rollout of those lifesaving injections.
The lack of planning and coordination. The insufficient workforce and training. The inadequate public messaging and outreach. And the failure to create a uniform database to track inventory and equitably distribute shots.
“We’re seeing the consequences now of a complete and utter failure to ensure we have a full and robust vaccination system,” Duchin said.
The chaotic execution of state and local vaccination programs is only the latest in a series of missteps by public health departments during the worst pandemic in more than a century. They include lackluster testing, contact tracing and data collection, and the failure to protect minority communities, which have borne the brunt of this disease.
All of those blunders, Duchin and other public health officials say, are a direct result of a decade of neglect of the nation’s public health system by both the federal government and state and local governments.
As state legislatures reconvene, lawmakers in many states will address immediate pandemic demands, such as vaccinations, testing and contact tracing programs. And some will work on measures designed to reopen schools safely. But most states, hamstrung by tight budgets, won’t be able to make the long-term investments needed to shore up their public health infrastructures.
In his State of the State address this month, New York Gov. Andrew Cuomo, a Democrat, vowed to create a state public health corps by working with Cornell University to train 1,000 public health fellows to assist in the immediate need to vaccinate state residents against COVID-19. California Democratic Gov. Gavin Newsom is proposing to spend $372 million in state funds to speed the delivery of COVID-19 vaccinations and $2 billion to ensure a safe return to K-12 in-person learning.
In Oregon, Democratic Gov. Kate Brown has proposed spending $30 million to modernize the state’s public health system. Next door in Washington state, Democratic Gov. Jay Inslee has proposed a budget that includes $397 million to pay for testing, personal protective equipment, lab costs, epidemiology work and vaccine distribution, and boost Washington’s public health system. And in Maine, Democratic Gov. Janet Mills wants to allocate $5 million to the Maine Center for Disease Control and Prevention for COVID-19 testing.
Some of the proposals could help public health agencies prepare for the next pandemic. But experts at the National Conference of State Legislatures predict that budget shortfalls will limit the number of states able to invest in emergency coronavirus funding, much less long-term development of public health infrastructure.
That bleak outlook stems from a web of challenges. Public health agencies must fill empty positions in a politically fraught environment, carry out a massive vaccination program that’s off to a rocky start and continue to manage ongoing crises such as substance use disorders and chronic diseases.
“In this country, policymakers tend to pay attention to public health when there is a crisis or an emergency,” said Dr. Ronald Valdiserri, a professor of epidemiology at Emory University’s Rollins School of Public Health and a former high-ranking official at the federal Centers for Disease Control and Prevention. “It may be human nature that too few policymakers can see beyond the short run, but public health requires a long-term vision, not just the next year or two and then move on to something else.”
We’re now paying the price for that neglect, Valdiserri and others said.
Paying the Price
When the coronavirus reached U.S. shores a little more than a year ago, a decade of short-term thinking, declining investment and boom-or-bust financing had already taken its toll. The nation’s more than 3,000 public health agencies were ill-prepared to protect Americans from an infectious disease that could only have been contained by a sustained, coordinated and well-resourced response.
Understaffed and hobbled by data systems that relied on telephones and fax machines to manage an avalanche of testing and new patient information, many state, city and county public health agencies fumbled.
Data systems varied widely, making it impossible to compare outbreaks and analyze the course of the disease.
Then, as the coronavirus crisis became the top political priority in every state, some governors and other elected officials sidelined public health officials and scientists, blamed them for unreliable data and made them scapegoats for unpopular COVID-19 restrictions, including school and business closures and mask mandates. In some places, local health officials faced death threats.
As a result, at least 181 public health officials have either resigned, retired or been fired since April 2020, according to an ongoing investigation by The Associated Press and Kaiser Health News.
Top public health officials have always had to make controversial decisions and they have always been criticized, said Dr. Georges Benjamin, executive director of the American Public Health Association. But never has the politicization of public health reached the local level, he said.
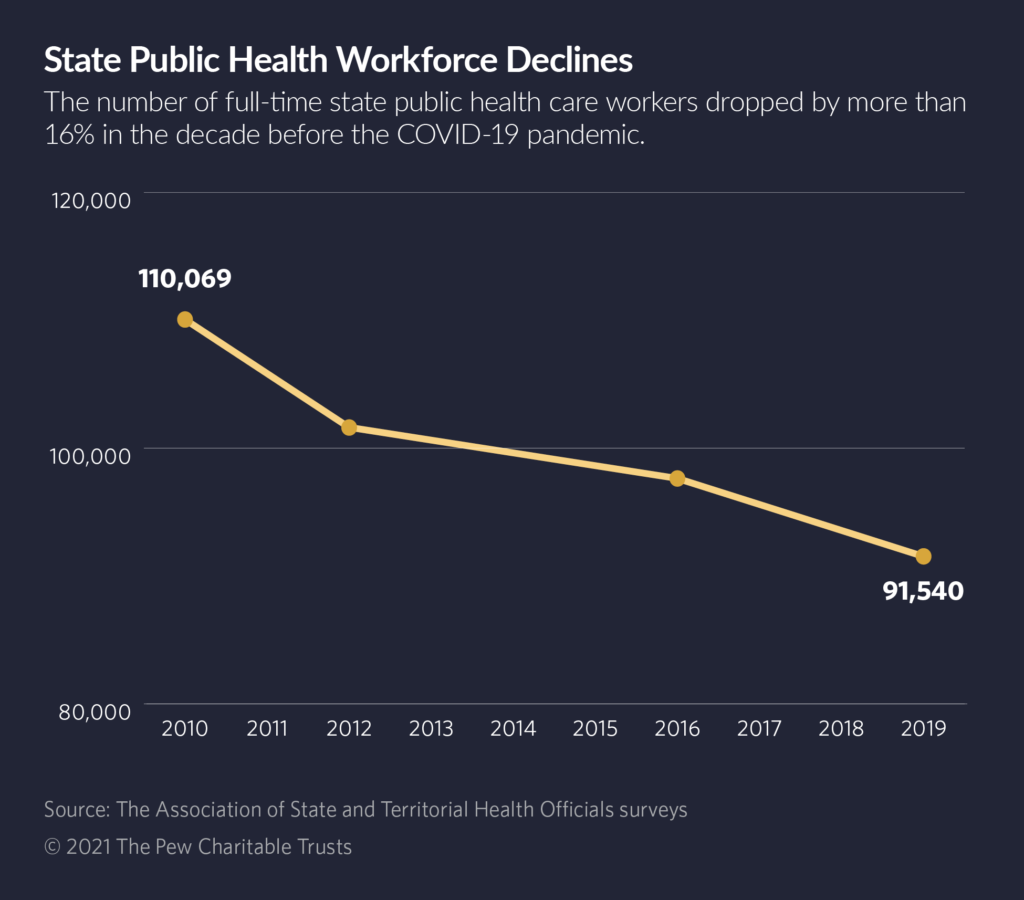
Agencies now are struggling to find a fresh bench of public health professionals in a field that has lost more than 56,000 positions in the past decade, according to the National Association of County and City Health Officials.
At the same time, they’re being asked to build the largest immunization program since the polio vaccination drive in the 1960s.
“It’s wonderful that new federal funding is coming in, but you can’t just hire new people on a dime,” said Jeffrey Levi, professor of health policy and management at the Milken Institute School of Public Health at George Washington University.
Defining Public Health
Public health is a poorly understood concept. At base, it refers to health care services that reach beyond a single individual to affect a neighborhood, community or population.
Public health services have been a staple of state and local government since the early 20th century. They range from broad childhood disease vaccination programs to basic medical services for people with no other access to health care.
Most local agencies also maintain surveillance systems to protect people from emerging infectious diseases, natural disasters, foodborne illnesses and toxic substances in air and drinking water supplies. They also educate the public on how to manage increasingly common chronic diseases such as diabetes and hypertension.
As new health concerns emerged, public health departments expanded their services. In the 1980s, public health took on the prevention and treatment of HIV/AIDS, and in the past decade, as opioid overdose deaths skyrocketed, local health agencies began distributing the overdose antidote drug Narcan.
But even when public health efforts are effective and well-regarded, they’re subject to the caprices of elected officials.
The money trail bears that out. Funding of public health initiatives through the years underscores the long-term underappreciation of the discipline. According to an analysis by the Association of State and Territorial Health Officials, state spending on public health fell by 22% between 2010 and 2018, while federal funding failed to keep pace with inflation.
Total state public health spending in 2018 was $24.5 billion, including funds received from the federal government. The Public Health Leadership Forum, among other public health organizations, says fully supporting core capabilities in public health would require an additional annual investment of $4.5 billion.
“What this pandemic has shown us is the singular importance of public health,” said former Pennsylvania health secretary Dr. Rachel Levine, who has been nominated by President Joe Biden as assistant secretary at the U.S. Department of Health and Human Services.
“We in public health have expressed concern about underfunding at the national, state and local level for many years, and our concerns were obviously well founded,” Levine said. “In the future, it will be critical, even as we get past COVID-19, to continue to fund improvements in the public health workforce, particularly in data management.”
Emergency Funding
To tackle the COVID-19 pandemic, the federal government is allocating about $22 billion in emergency funds to threadbare state and local public health agencies, by way of a congressional bill passed in December. Prior to that, Congress appropriated roughly $35 billion for public health-related pandemic activities, bringing total federal grants to state and local public health agencies to more than $57 billion for 2021.
Biden has proposed $160 billion in additional public health spending as part of a $1.9 trillion pandemic stimulus package. That funding would bolster the administration of vaccines, improve contact tracing and address the disparities in health outcomes experienced by minority communities during the crisis. It also would include the addition of 100,000 public health workers.
This pattern is a familiar one in public health, said Michael Fraser, executive director of the Association of State and Territorial Health Officials. When a public health emergency hits, funding flows, only to disappear again when the threat subsides.
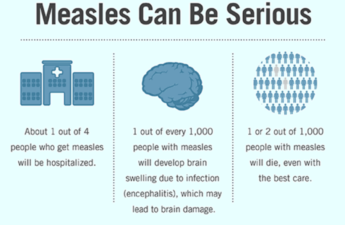
“We’ve told this story before but not at this scale,” Fraser said. “Prior to COVID, there was the measles outbreak and prior to that was Zika. There are many examples.”
The same pattern, public health officials say, occurred after 9/11 when fears arose over biomedical threats, and after the H1N1 flu outbreak of 2009.
“We have members of Congress elected for two years or six years. There’s a very short-term memory on the Hill,” Fraser said.
Lawmakers have continued this pattern of inconsistent, disaster-related funding despite alarms from public health officials for more than a decade about the burgeoning threat of a pandemic.
Similarly, in the face of more frequent hurricanes, wildfires, tornadoes and other natural disasters, elected officials have meagerly responded to public health officials’ pleas for permanent preparedness funding.
When a crisis strikes, Seattle’s Duchin said, public health agencies are forced to move staff from other essential services to meet the emergency of the moment until new funding starts to flow.
That happened during COVID-19: Duchin said he had to put previously identified priority areas, such as the spread of hepatitis A and hepatitis C, as well as salmonella, hospital mold and multidrug resistant organisms, on hold, and move workers to COVID-19 testing and contact tracing.
Even when money is allocated from the federal government, it is typically designated for specific diseases. Those restrictions curb local agencies’ flexibility to prioritize their jurisdictions’ needs, he said.
Baltimore Health Commissioner Dr. Letitia Dzirasa gave the example of funding for HIV/AIDS, most of which comes to the city by way of the federal Ryan White program to provide treatment. If the city had the freedom to spend some of that funding on education and prevention, she said, it could more effectively root out the disease. The specificity of the funding, she said, “prevents us from taking a more holistic approach.”
Much of the public health funding states receive comes from the Centers for Disease Control and Prevention. A 2020 report from the Trust for America’s Health, a nonpartisan group advocating for universal health access, argues that a lack of money has impaired one program after another, from emergency preparedness to chronic disease prevention to stemming the use of deadly synthetic opioids such as fentanyl.
“Under current funding,” the Trust for America’s Health report said, “CDC cannot provide adequate resources to all eligible states or communities, leaving many underfunded or unfunded for certain prevention activities, which harms health and exacerbates health disparities.”
A 2018 survey conducted by public health researchers found that only half of Americans live in an area with a full array of public health services.
Lori Tremmel Freeman, CEO of the National Association of County and City Health Officials, said she’s hopeful the pandemic will raise awareness in Congress and state capitols of the need for adequate and consistent public health funding.
The pandemic exposed the consequences of the nation’s failure to invest in core public health functions that would have armed states and cities to combat the virus.
At the same time, the disproportionate rates of illness and death among Black, Latino and Native American people laid bare the inadequacy of another essential public health function—addressing the social determinants of health, including poor access to health care, transportation and employment, and inferior housing.
“The communities most harmed by the virus are the communities that already suffered the most from chronic diseases and other underlying conditions. They did not necessarily have to suffer more,” Freeman said. “As a country we have the ability to ensure that in the future people have what they need to be healthy.”
<p style="text-align: center;"><a href="http://www.pewstates.org/projects/stateline"><img class="alignnone wp-image-30206 size-full" src="http://mylocalhealthguide.com/wp-content/uploads/2013/04/Stateline-logo.jpg" alt="Stateline logo" width="948" height="199" /></a> Stateline is a nonpartisan, nonprofit news service of the Pew Center on the States that provides daily reporting and analysis on trends in state policy.</p>