Stephen Kent, The University of Melbourne
COVID is rampant in many parts of the world right now. Some people battling or recovering from infection may wonder if catching COVID will give them longer term immunity for when the next wave comes.
Since the early days of the pandemic we’ve known COVID induces a wide range of immune responses and one infection provides partial protection from future infections.
Unfortunately, immunity wanes over time – people lose half their immunity every 3 months. Further, new variants continue to emerge that are partially resistant to key immune responses – antibodies that neutralise earlier strains – this is especially true of Omicron.
We’re starting to get a more detailed understanding of COVID immunity across variants. Here’s what we know so faros . . .
Breakthrough infection happens but vaccines are still a must
Since around 95% of Australians over 16 have had at least two COVID vaccines, most people catching COVID now have previously been vaccinated – this is called “breakthrough infection”.
The vaccines are effective at substantially reducing severe COVID illness. They are less effective, particularly over time, at preventing infections, including with new variants. A third vaccine dose helps maintain immunity, and everyone eligible should get a booster as soon as possible.
Because the Astra-Zeneca vaccine is less effective than the Pfizer or Moderna vaccines, it’s critically important for vulnerable older Australians immunised with two Astra-Zeneca vaccinations to be boosted with a third vaccine dose as quickly as possible.
The good news is people first vaccinated with Astra-Zeneca and subsequently boosted with Pfizer or Moderna develop high levels of protective immune responses.
Recent work shows a nice boost in antibody immunity after breakthrough infection. This boost in antibody immunity may not be as fast or strong as getting a vaccine, but it has a big advantage in that the immunity is more specific to the infecting strain such as Delta.
The current vaccines are still based on the original strain isolated in Wuhan, China in early 2020. Several vaccine manufacturer’s are racing to update their vaccines for the Omicron variant (much as we do with the yearly flu vaccines), but these variant-specific vaccines are still some months away.
Infection immunity builds where COVID strikes first
Another potential advantage for immunity derived by infection (acquired in the respiratory tract) compared to vaccination (given into the muscle) is that immunity is better focused to the surfaces of the nose, throat and eyes. This is where COVID is first encountered.
Surface antibodies (termed immunoglobulin A) and specialised tissue “resident” immune cells (B and T-cells) are induced by infection but not intramuscular vaccination.
The level of protection offered by these “local” or “mucosal” responses is not yet clear in people, but some studies in animal models suggest they are helpful.
Delta infection offers a little protection against Omicron
The Omicron variant is slowly replacing the Delta variant around the world. It is more transmissible and avoids antibodies more effectively.
Do people who have been infected with the Delta variant have an advantage in terms of protection from the Omicron variant? The two strains share some sequence changes, but Omicron has many more mutations than Delta.
Only a minority of neutralising antibodies that fight Delta can also neutralise the Omicron variant. That said, neutralising antibodies against Delta are better at fighting Omicron than previous strains. This is particularly true for people who have caught Delta and been previously vaccinated.
The reverse is also true – people who have caught Omicron have some improved antibody protection against Delta. This may not be much use as Delta is disappearing from prevalence, but the knowledge could be useful for future variants.
T-cells might be key to cross-variant protection
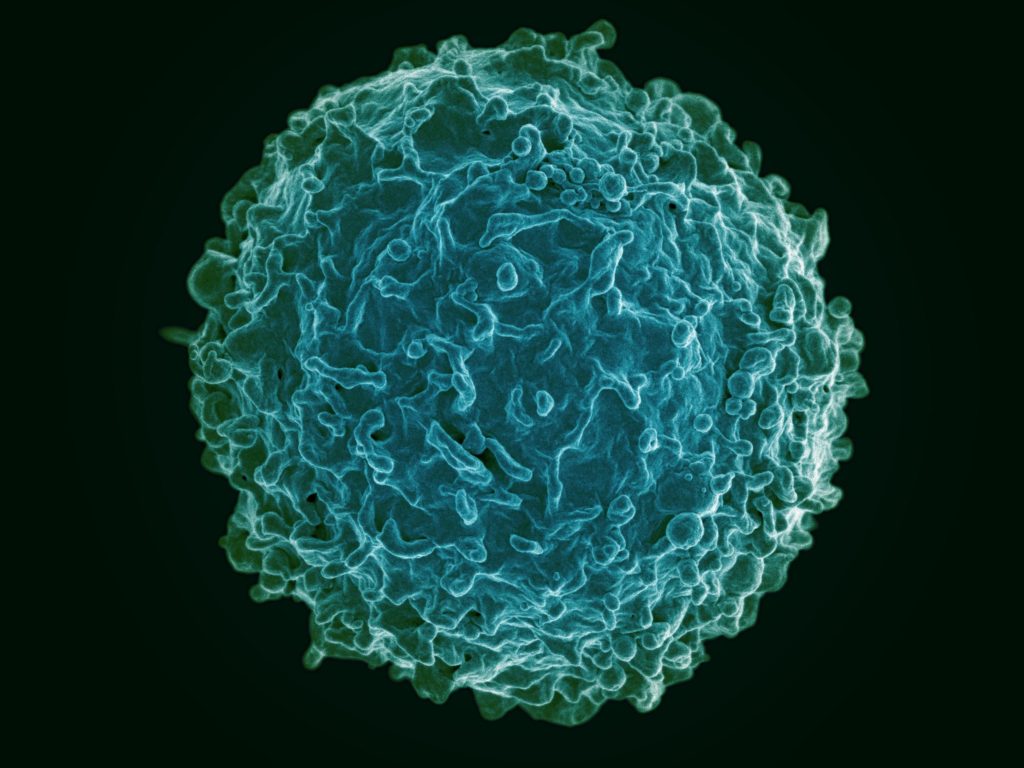
There is considerable interest in a type of immunity called T-cells and their potential ability to fight COVID infection.
Theoretically, T-cells could assist in protecting against severe infection with new strains because T-cells usually cross react to all variants of SARS-CoV-2, the virus that causes COVID.
However, the evidence to date points to the central role of neutralising antibodies obtained from infection or vaccination in protection from both getting an infection and preventing severe disease. A recent unpublished study suggests neutralising antibodies are boosted by breakthrough infections but not T-cells. We know T-cells are very important in protecting from other infectious diseases and many cancers, but perhaps have a lesser role in COVID.
Gaining immunity isn’t the end of the story
Overall, infections with Delta and Omicron provide a boost in immunity against these strains. Infection will probably help protect individuals from reinfection with the same variant. Infection may offer a small amount of protection from different variants and potentially from future variants.
However, immunity will not be enduring and it is still possible to get severe infections and ongoing symptoms (termed “Long COVID”) from breakthrough infections. They are best avoided! Current booster vaccines along with social measures are our best way to stay healthy while we wait for Omicron-specific vaccines.
Stephen Kent, Professor and Laboratory Head, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license.
Read the original article.


