Duncan Robertson, Loughborough University
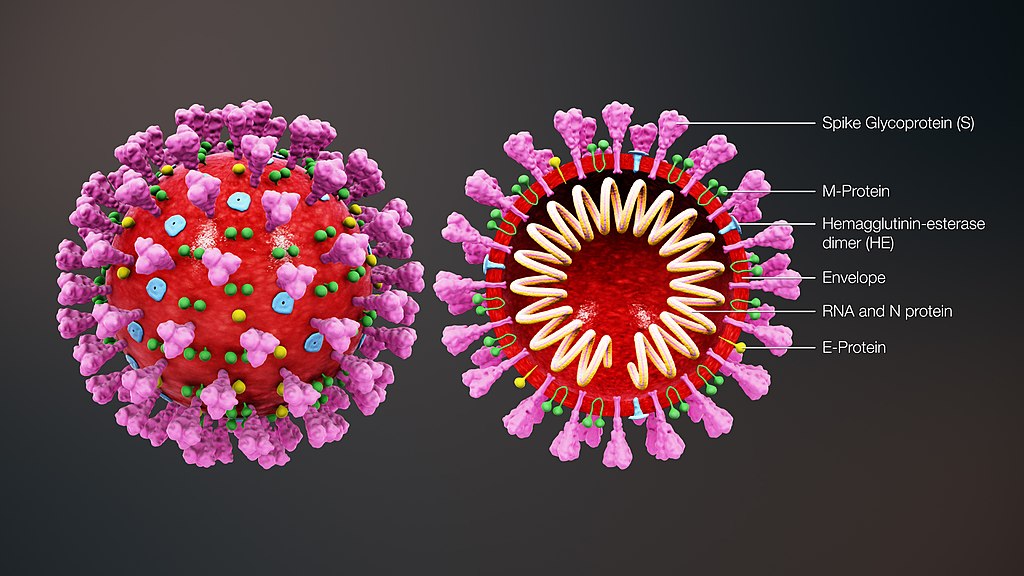
In 2020, we knew very little about the novel virus that was to become known as COVID-19. Now, as we enter 2023, a search of Google Scholar produces around five million results containing the term.
So how will the pandemic be felt in 2023? This question is in some ways impossible to answer, given a number of unknowns. In early 2020 the scientific community was focused on determining key parameters that could be used to make projections as to the severity and extent of the spread of the virus. Now, the complex interplay of COVID variants, vaccination and natural immunity makes that process far more difficult and less predictable.
But this doesn’t mean there’s room for complacency. The proportion of people estimated to be infected has varied over time, but this figure has not fallen below 1.25% (or one in 80 people) in England for the entirety of 2022. COVID is very much still with us, and people are being infected time and time again.
Meanwhile, the number of people self-reporting long COVID symptoms in the UK is around 3.4%, or one in 30 people. And the cumulative risk of acquiring long COVID grows the more times people are reinfected with COVID.
The UK’s health system is under huge pressure, with very high pre-COVID waiting times having been exacerbated during the pandemic.
Why COVID projections have become harder
During the early days of the pandemic, simple models could be used to project the number of COVID cases and the likely effect on the population, including demands for health care.
Relatively few variables were needed to produce the first projections. That was because there was one main variant of COVID, the original strain, to which everyone in the world was susceptible.
But now, those simple assumptions no longer hold. Much of the world’s population is estimated to have had COVID and there are significant differences between individual levels of protection in terms of which vaccines, and how many doses, people have received around the world. In total, 13 billion vaccine doses have been administered – but not equitably.
Modelling also works well when people act in ways that are predictable, whether this is normal, pre-pandemic behaviour, or at times of severe social restrictions. As people adapt to the virus and make their own assessment of risk and benefits of behaviour, modelling becomes more complex.
A reduction in surveillance also makes modelling more difficult. During the peak of the emergency response to COVID this was a priority, including surveillance of people with the virus, and surveillance of variants. This allowed new variants such as omicron to be identified early and responses to be prepared.
The UK in particular produced two million COVID sequences up to February 2022, accounting for one-quarter of the world’s genome sequencing output. But sequencing activity has subsequently decreased, which may increase the time it takes to identify new variants of concern.
The pandemic is not over
There remain big differences in pharmaceutical and non-pharmaceutical interventions in place around the world, for example the use of masks, COVID testing and building ventilation. As governments loosen and at times re-tighten their responses to react to dynamic medical and social pressures, there is a risk that variants could emerge which evade some of the defences that populations have built up.
The next stages of the pandemic will also be influenced by people’s behaviour. For instance, how much we work from home and whether we reduce our social contacts when infectious.
There’s no certainty that new variants will emerge that have an effect in the order of delta or omicron, but it is possible. Should this occur, it’s important that plans are in place to respond in the context of waning interest in COVID and resurgent misinformation and disinformation.
Beyond 2023 – the next pandemic
It’s pertinent to ask how much learning has taken place during the COVID pandemic to improve the response to the next pandemic.
During this pandemic, we’ve often seen short-term national interests prioritised, with a focus on national responses to vaccine equity while discounting the long-term global availability of vaccines. While laudable initiatives such as Covax were established, conceived to provide equitable access to COVID vaccines and treatments, the challenge is to design incentives for nations to cooperate to reduce long-term global risks.
As with any political response, the priorities of the emergency phase can all too easily be forgotten, such as governments’ abilities to manufacture vaccines. The UK government’s sale of the Vaccine Manufacturing and Innovation Centre is an example of this. Capacity to develop and produce vaccines quickly would stand us in good stead for the next pandemic, but these priorities now have to compete against others that are more immediate or politically expedient.
The UK’s COVID inquiry is bound to be presented with thousands of pages of evidence, with many submissions giving clear, self-consistent accounts of “lessons learned”. Whether those lessons are put into practice is another matter entirely.
Duncan Robertson, Senior Lecturer in Management Sciences, Loughborough University
This article is republished from The Conversation under a Creative Commons license.
Read the original article.